Five facts about physiotherapy and functional neurological disorder
Five discussion points about physiotherapy for people with functional neurological disorder are explored by Anna Jones, Daniel Luther, Dharsha Petrie, Rielan Newell and Sara Issak of the APA Neurology national group.
FND is diagnosed with positive clinical signs
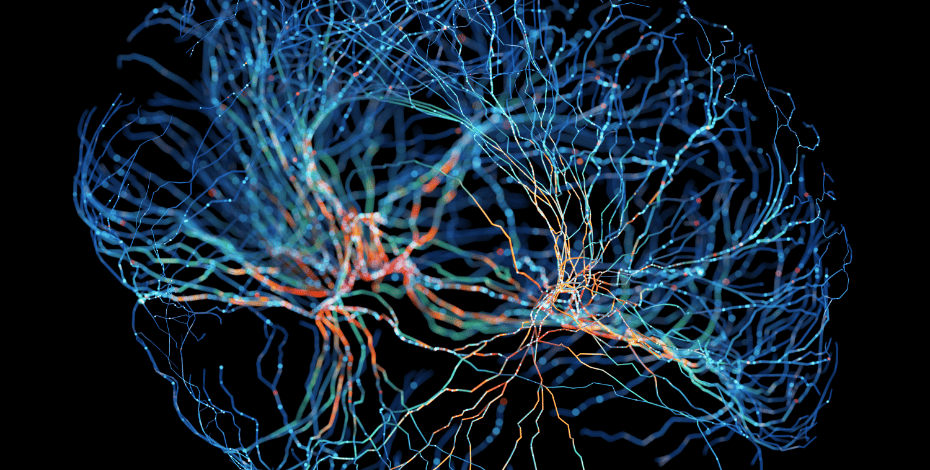
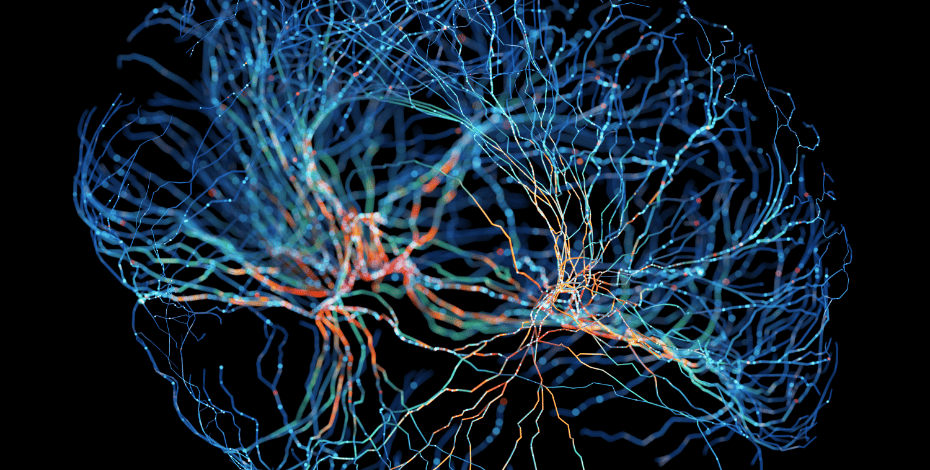
Functional neurological disorder (FND) is characterised by involuntary movements and other symptoms that arise from a disruption to how the brain processes information, rather than from structural damage to the brain or nervous system itself.
The brain processing information.
FND is a diagnosis of inclusion, made using positive clinical signs in combination with effective history taking (Stone et al 2024).
Positive clinical signs include the Hoover’s sign, used to detect functional leg weakness, and the tremor entrainment test, which assesses whether tremors will synchronise with voluntary rhythmic movements in another body part (Bennett et al 2021).
Such signs are reproducible and distinguish FND from other neurological conditions, enhancing diagnostic confidence.
Diagnosis accuracy is similar to conditions such as Parkinson’s disease.
The aetiology of FND involves complex interactions between biological, psychological and social factors.
Functional imaging studies suggest altered brain activity in areas such as the supplementary motor area and anterior cingulate cortex, which are involved in movement and attention regulation (Espay et al 2018).
These findings support our understanding of FND as a genuine neurological condition rather than a purely psychogenic disorder, countering historical misconceptions.
By focusing on positive signs and neurobiological underpinnings, clinicians can provide effective explanations and education, enabling tailored treatment plans and improved outcomes for patients with FND.
FND is common, disabling and costly
FND is a prevalent and debilitating condition.
FND places a high burden on the healthcare system.
It affects an estimated four to 12 people per 100,000 annually and represents 15 per cent of diagnoses given to patients in outpatient neurology settings in Australia (Ahmad & Ahmad 2016).
According to Carson et al (2011), it is the second most common reason for someone to seek a neurology consultation.
It can be severely disabling, affecting quality of life and daily functioning, and symptoms often persist in the long term (Gelauff et al 2014).
High rates of unemployment and social isolation have been reported, comparable to those in people with other neurological conditions such as multiple sclerosis and epilepsy (Carson et al 2011).
FND places a significant financial burden on the Australian healthcare system.
Although specific national cost data is limited, studies suggest high direct healthcare costs due to misdiagnosis, recurrent medical consultations and repeated investigations (Pepper et al 2022).
A 2019 Australian study found that individuals with FND frequently utilise emergency services and outpatient care and are often admitted to hospital (Gill 2019).
These interactions often arise from diagnostic delays and an absence of dedicated therapy services.
Research highlights the need for efficient diagnosis and better access to treatment services to reduce long-term costs (Gill 2019).
FND recovery requires coordinated, multidisciplinary care
FND is a multifaceted condition whose symptoms extend beyond abnormal movements.

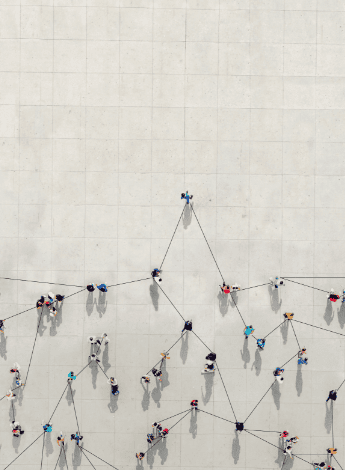
FND requires coordinated help.
These include fatigue, chronic pain, seizures, vision changes and urinary or bowel disturbances (Gilmour et al 2020).
Successful management often requires both physical and psychological therapies, with evidence supporting approaches like physiotherapy (Nielsen et al 2013, Nielsen et al 2024), psychology (Goldstein et al 2020, Van Patten & Bellone 2023) and other allied health (Baker et al 2021, Nicholson et al 2020).
Although further research is needed on how rehabilitation is delivered (Polich et al 2022), significant functional improvements have been enabled by existing FND inpatient models focused on rehabilitation (Czarnecki et al 2012, Saunders et al 2024).
This is alongside multidisciplinary FND outpatient models of care (Guy et al 2024, Petrochilos et al 2020) and virtual care (Demartini et al 2020, Perez 2021).
However, many care models lack true collaboration between specialties, with disciplines often working independently rather than collaboratively (Lidstone et al 2020).
Forming an integrated treatment team may help bridge the gap between mind and body, fostering validation and alignment within the care process by reflecting this integration within the team dynamic itself (Lidstone et al 2020).
Physiotherapists' key role in FND management
Physiotherapists play a pivotal role in managing FND through targeted strategies that address core symptoms, movement and participation in daily life.

Task-oriented exercises can help.
Education is an essential component. It allows patients to understand that FND is a potentially reversible biopsychosocial condition caused by nervous system dysfunction rather than damage (Nielsen et al 2015, Stone 2009).
Physiotherapists promote self-management by identifying treatment goals, setting achievable milestones and encouraging independence.
Focusing on attentional shift strategies, physiotherapists employ cognitive and other sensory-level distractions such as engaging patients with familiar conversations, music or mental tasks.
Task-oriented exercises, however, are often more effective because they promote implicit motor control and functional improvements (Nielsen et al 2015).
Familiar tasks provide effective and personalised distractions to divert attention away from symptoms.
Additional strategies include improving routines and physical activity with graded non-specific exercise to prevent fatigue and overexertion, fostering confidence and gradual functional recovery (Dallocchio et al 2010, White et al 2011).
A symptom management plan prepares patients to handle symptom exacerbations with relaxation techniques, pacing and activity modifications.
Balance and gait retraining emphasises automatic and task-specific movements to restore mobility while incorporating the attentional shift strategies.
Collectively, these approaches empower patients to regain functional control and improve their quality of life.
Physiotherapists can advocate for patients with FND
Diagnosing someone with FND is a critical first step. A clear and confident diagnosis, along with a thorough explanation, can be therapeutic in itself and facilitates evidence- based, interdisciplinary care (Stone et al 2016).

Physios can advocate for patients with FND.
Physiotherapists can play a key role in advocating for the timely diagnosis of FND.
As experts in the structure and function of the human body, we are well positioned to identify symptoms and signs that may indicate FND.
Early referral to a neurologist offers the person an opportunity for a diagnosis; timely and accurate diagnosis is essential because
a delayed diagnosis is associated with poorer outcomes, including prolonged symptoms and increased disability (Gelauff & Stone 2016).
FND is poorly understood by both the general public and healthcare professionals, with high levels of stigma (Gill 2019).
At the same time, access to neurologists is limited in Australia, particularly in rural and regional areas (Simpson-Yap et al 2023).
This highlights the need for strong advocacy on behalf of individuals with FND, but to advocate effectively, we need a good understanding of positive clinical signs and diagnostic criteria.
Consensus recommendations for physiotherapy management and resources such as FND Australia (fndaustralia.com.au) and FND Guide (neurosymptoms.org) are a good starting place to help us learn to better identify, advocate for and manage FND.
>> Anna Jones APAM is a neurological physiotherapist and the clinic manager of Advance Rehab Centre Artarmon. Anna has a strong interest in FND and in educating other allied health professionals about FND. She is a member of the APA Neurology group.
>> Daniel Luther APAM is a senior neurological physiotherapist at John Hunter Hospital. Over the past five years, Daniel has been working with an interdisciplinary team to improve the management of FND patients. He is a member of the APA Neurology group.
>> Dharsha Petrie MACP is an APA Titled Neurological Physiotherapist and an advanced physiotherapist at the Surgical, Treatment and Rehabilitation Service in Brisbane. Dharsha has an interest in neurological rehabilitation including for stroke, traumatic brain injury and movement disorders. She is the national chair of the APA Neurology group.
>> Rielan Newell APAM is a senior outpatient neurological physiotherapist and hospitals manager at Active Rehabilitation Physiotherapy in South Brisbane, which services the Mater Private Hospital and Brisbane Private Hospital. Rielan has an interest in FND and is a member of the APA Neurology group.
>> Sara Issak APAM is a senior physiotherapist working in outpatient neurological rehabilitation at Epworth HealthCare, including
in the Epworth FND clinic. Sara is currently completing a PhD at the University of Melbourne, investigating the characteristics of functional gait disorders. She is a member of the APA Neurology group.
QUICK LINKS
COURSE OF INTEREST
Awareness of possible functional neurological symptom disorder in physiotherapy clinical practice
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.