
Five facts about enhanced recovery after joint replacement

Emma Blake, Larissa Sattler, Caitlin Stark, Lucy Haydock and Thomas Petrie of the APA Orthopaedic national group present five discussion points on multidisciplinary approaches to joint replacement surgery and recovery and their effect on preoperative and postoperative physiotherapy.
1. Joint replacement recovery benefits from ERAS programs
Enhanced recovery after surgery (ERAS) is a multidisciplinary pathway encompassing key recommendations for the management of major surgery.
In 1995, Danish surgeon Professor Henrik Kehlet outlined this multimodal approach to recovery in order to improve the surgical stress response following colon resection surgery.
This was achieved through minimally invasive surgical techniques, regional anaesthesia and early nutrition and mobilisation.
These protocols have developed over time to include pathways for other major surgeries, including urological, bariatric, liver and joint replacement surgery.
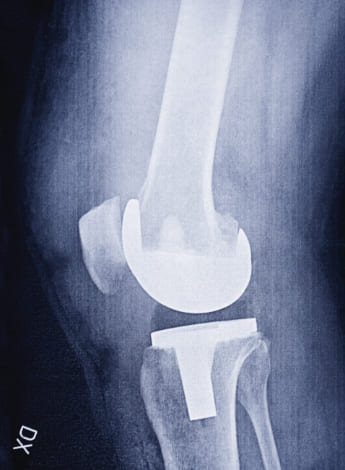
There is increasing demand for joint replacement surgery due to the growing burden of hip and knee osteoarthritis.
Meeting this demand requires safe and efficient models of care (Ackerman et al 2023).
ERAS pathways after joint replacement surgery are designed to reduce length of stay through evidence-based interventions including preoperative optimisation, perioperative management, postoperative analgesia, early mobilisation and criteria-led discharge.
There is evidence to suggest that ERAS protocols can improve patient outcomes and reduce healthcare costs without significant harm.
This includes reoperations, blood transfusion rates, hospital readmissions, infections, wound complications, periprosthetic fractures, venous thromboembolism, dislocations and mortality (Berkovic et al 2023).
In 2020, the ERAS Society published a consensus statement with recommendations for perioperative care of patients undergoing total hip and knee replacement surgery within an ERAS program (Wainwright et al 2020).
2. Prehabilitation may optimise postoperative recovery

The preoperative phase of an ERAS pathway commonly includes patient education as well as physical and psychological optimisation for surgery, often referred to as prehabilitation (Kaye et al 2019).
Prehabilitation aims to optimise the functional status and psychological readiness of patients prior to surgery to improve postoperative outcomes (Cabilan et al 2015, Hines & Munday 2015).
Existing protocols vary in type and intensity, predominantly focusing on exercise, including aerobic exercises, lower limb strength training, flexibility exercises, balance training and functional task activities (Moyer et al 2017).
Current preoperative usual care consists of general surgical advice and encouragement to remain physically active.
However, the results of research comparing usual care to an exercise-based prehabilitation program are contradictory (Punnoose et al 2023).
There is also increasing recognition of the benefits of including lifestyle modifications in traditional exercise-based prehabilitation (Richey et al 2020, Seward & Chen 2022).
Lifestyle modifications often include weight loss, disease education, pain coping strategies, cognitive behavioural therapy, stress management, mind–body interventions and behaviour change (ie, smoking and alcohol secession) (Fecher-Jones et al 2021, Sattler et al 2023).
With growing support for the addition of lifestyle modifications to a prehabilitation protocol, future prehabilitation research that includes physiotherapy should consider incorporating them.
A more standardised approach to reporting prehabilitation interventions within the literature is also needed to thoroughly evaluate the effects of prehabilitation on postoperative outcomes.
3. Perioperative and intraoperative factors play an important role in ERAS

Minimally invasive surgical techniques aim to reduce blood loss, wound size and disruption to soft tissues, thereby reducing pain and improving function earlier in recovery for a reduced length of stay.
However, there is no consensus on the approach to lumbar spine surgery and conflicting evidence for a direct anterior approach versus a posterior or lateral approach in total hip replacement (Debono et al 2021, Wainwright et al 2020).
There is also a paucity of evidence for the muscle-sparing mini-subvastus approach to total knee arthroplasties; more comprehensive research is based on the standard medial parapatellar approach (Geng et al 2022, Gromov et al 2017).
Wainwright’s 2020 guidelines suggest that no one approach can presently be recommended.
Traditional fasting from midnight has not been shown to reduce risk for patients and ERAS guidelines support reducing fasting times for solids to six hours and for clear fluids to two hours.
This is designed to negate the catabolic state caused by surgery that negatively affects healing (Jankowski 2017, Wainwright et al 2020).
Optimising fluid balance and minimising blood loss improve wound healing and reduce the need for allogenic transfusion—the use of tranexamic acid is the most supported method here, including in lumbar fusion (Kaye et al 2019, He et al 2020).
4. Anaesthetics help patients access timely postoperative physiotherapy

Anaesthetics play a key role in recovery, especially in the orthopaedic setting.
The management of analgesia, postoperative nausea and vomiting and return of function after motor blockade affects the ability to provide timely postoperative physiotherapy according to the current ERAS recommendations.
Short-acting spinal anaesthetics and intraoperative local anaesthetics are the preferred methods for ERAS.
Limiting the use of volatile anaesthetics and opting for adjunct therapies such as perioperative nerve blocks or neuraxial anaesthetics can reduce the need for opioid analgesics and allow quicker return of function following neuromuscular blockade (Tippireddy & Ghatol 2024).
Postoperative nausea and vomiting prophylactic measures have been found to have an impact on patient experience and length of stay (Tippireddy & Ghatol 2024).
Common agents in preventing postoperative nausea and vomiting include antibiotics, antiemetic therapies (dimenhydrinate, dexamethasone, ondansetron and propofol) and opioid avoidance (through the use of paracetamol, non-steroidal anti-inflammatories, steroids and tapentadol).
Euvolemia (maintaining normal fluid balance) is vital for optimising tissue healing in the perioperative to postoperative phase.
Both hypovolaemia and fluid overload can have an effect on postoperative complications and patient survival.
Goal-directed therapy or zero-balance therapy are thought to have the best patient outcomes (Scott & Miller 2015).
5. Patients should be mobilised early after joint arthroplasty
Early mobilisation after elective orthopaedic surgery is safe and may facilitate accelerated patient recovery.

Recent guidelines recommend that patients be mobilised as soon as possible after surgery (Wainwright et al 2020).
There is level 2 evidence that early mobilisation after lower limb arthroplasty and lumbar spinal fusion surgery can reduce hospital length of stay with no significant difference in perioperative morbidity, immediate adverse outcomes or readmission rates (Morrell
et al 2021, Okamoto et al 2016).
Early mobilisation can counteract the adverse effects of prolonged bed rest, such as an increased risk of thromboembolism, muscle atrophy, reduced pulmonary function, compromised tissue oxygenation and insulin resistance (Wainwright et al 2020).
Due to advancements in perioperative care, postoperative patients now have fewer medical attachments, which can make mobilisation easier.
Current guidelines do not recommend the routine use of urinary catheters or wound drainage after lower arthroplasty or short-segment lumbar spine fusions, with or without decompression (Debono et al 2021, Wainwright et al 2020).
The ERAS Society strongly recommends criteria-based discharge pathways to facilitate direct discharge home.
Following hip and knee arthroplasty, this might include independent mobility with a walking frame or crutches and independence with bed transfers, with rising from a chair or toilet and with dressing and personal care (Wainwright et al 2020).
Quick Links:
Course of interest:
>> Emma Blake APAM is a senior physiotherapist in orthopaedics at Hollywood Private Hospital, Perth, and the national chair of the APA Orthopaedic group. With a keen interest in pain management and complex revision joint replacement surgery, Emma helped establish an inaugural accelerated joint replacement rehabilitation program.
>> Dr Larissa Sattler APAM is an assistant professor within the Doctor of Physiotherapy program at Bond University, Gold Coast. Larissa completed a PhD on advancements in total knee replacement rehabilitation and is actively involved in a number of orthopaedic research projects. She is a member of the Orthopaedic group.
>> Caitlin Stark APAM has a keen interest in the preoperative, perioperative and postoperative management of orthopaedic patients, particularly joint replacement patients. Caitlin is currently working privately for Associate Professor Kaushik Hazratwala in a care coordination, physiotherapy and organisational role. She is a member of the Orthopaedic group.
>> Lucy Haydock APAM works as a physiotherapist at the Princess Alexandra Hospital in Brisbane. Lucy has a special interest in orthopaedics and musculoskeletal physiotherapy. She is a member of the Orthopaedic group.
>> Thomas Petrie APAM is a senior physiotherapist in orthopaedics at the Princess Alexandra Hospital. Thomas has had extensive experience in elective, trauma and reconstructive orthopaedics at the Nuffield Orthopaedic Centre, Chelsea and Westminster Hospital and the Royal London Hospital, UK. He is the Queensland chair of the Orthopaedic group.
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





