
Five facts about suicide prevention in physiotherapy

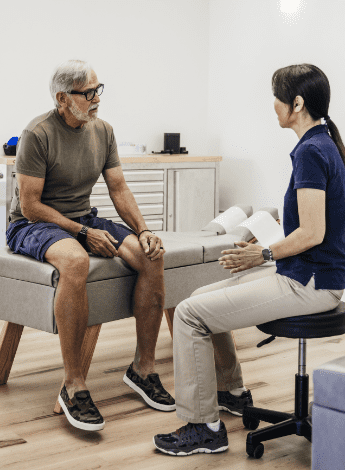
Strategies for recognising suicidality and contributing to suicide prevention are within the scope of physiotherapy. Ellen Lake, Ryan McGrath and Sophie Shephard present five discussion points about suicide prevention in a clinical context.
1 Suicide prevention is everyone’s business

Mental health is one of Australia’s most pressing issues and there is an urgent need for a skilled and contemporary mental health workforce (Australian Government n.d.).
As well as people who work exclusively within the mental health sector, this workforce needs to include those who work in other healthcare settings who ‘frequently treat, interact with, care and support people experiencing suicidality, mental distress and/ or ill-health’ (Australian Government n.d.).
Broadening the scope of suicide prevention to include additional community touchpoints offers significant benefits, including reaching individuals who may not otherwise seek help or have ready access to clinical mental health services (Morse et al 2019).
Healthcare settings in general provide an opportunity for creating environments that encourage help-seeking behaviours (Gallagher et al 2023).
Although physiotherapy may not be the first health profession that comes to mind for suicide prevention, physiotherapists are in a position to play a vital role in this crucial area (McGrath et al 2023).
Physiotherapists commonly support people experiencing chronic physical illness, injury and disability—identified as priority population groups by Suicide Prevention Australia (McGrath et al 2024, Suicide Prevention Australia 2023a).
Physiotherapists are skilled at forming strong relationships with clients, families, carers and their local community (Tasker et al 2012).
These relationships mean that clients may feel comfortable disclosing thoughts of suicide to them (McGrath et al 2020).
2 One in two physiotherapists report receiving disclosure of a suicide plan
A recent survey of 338 Australian physiotherapists revealed that nearly half had received at least one disclosure of a suicide plan during their career (McGrath et al 2024).
This was not an unexpected finding; poor physical health is a risk factor for suicide.
People who frequently engage in self-harm and suicidal behaviour not only face significant mental health challenges but also often experience chronic physical illnesses and pain (Sadath et al 2023).
For example, nearly 50 per cent of people with chronic pain have thought about suicide and approximately 20 per cent of people who identify as male or non-binary and live with chronic pain have made a plan for suicide (Chronic Pain Australia 2024).
A diagnosis of severe conditions is also linked to a heightened risk of suicide.
Among individuals diagnosed with a degenerative neurological condition, the one-year suicide rate was 114.5 per 100,000, much higher than the rate of approximately 9.2 per 100,000 in the general population (Nafilyan et al 2023).
3 Suicide prevention strategies the workplace

There are strong links between employment and mental health.
Employment lowers the overall risk of suicide (Kinchin & Doran 2017).
It helps to shape a person’s sense of identify through feelings of worth, belonging and connection and offers the opportunity for meaning and purpose, structure, ritual and financial and accommodation stability (Kinchin & Doran 2017).
Disruption to a sense of self can occur through injury, illness, disability, family and relationship breakdown, and legal and financial strains. These disruptions can happen to any worker in any workplace setting.
Suicide prevention competency frameworks within the workplace help to build the capacity and capability of the clinical workforce in responding to people experiencing suicidal thoughts and behaviours (Suicide Prevention Australia 2023b).
Barriers to implementation of frameworks include leadership buy-in, funding shortfalls and time constraints.
Internationally recommended workplace practices that support suicide prevention include leadership and care culture, job strain reduction, communication and reduction of stigma, self-care orientation, training, peer support and wellbeing ambassadors, mental health and crisis resources, mitigating risk and crisis response.
4 Physiotherapists can act as LifeKeepers
Physiotherapists’ frequent contact with individuals experiencing suicidal thoughts and behaviours presents an opportunity for them to act as a vital link between physical and mental health services (McGrath et al 2023).
LifeKeepers, also known as gatekeepers, are individuals equipped with the awareness, confidence, skills and knowledge to identify those experiencing suicidal thoughts and behaviours and to connect them with appropriate support (Hawgood et al 2021, Roses in the Ocean n.d.).
Being a LifeKeeper is not limited to mental health professionals (Hawgood et al 2021).
Anyone, including sports coaches, taxidrivers and hairdressers, can serve as a LifeKeeper (Roses in the Ocean n.d.).
In addition to acting as LifeKeepers, physiotherapists can work towards addressing the determinants of suicidal thoughts and behaviours.
By helping individuals manage their physical health conditions, they can contribute to reducing suicidal thoughts and behaviours (McGrath et al 2023).
For example, a meta-analysis has shown that while exercise does not significantly reduce suicidal ideation, it does significantly reduce suicide attempts.
This finding underscores the multifaceted role physiotherapists can play in suicide prevention (Fabiano et al 2023).
5 Suicide prevention is supported

Many physiotherapists express an interest in tailored training in suicide prevention (McGrath et al 2021, McGrath et al 2020) and a strong desire to care for the physical and mental wellbeing of their clients (Lunden & Bergenheim 2020).
There are basic competencies in this area that are well within the scope of physiotherapy, such as the ability to recognise suicidality (including warning signs), knowledge of local referral resources and the ability to engage and connect with the person experiencing suicidal thoughts and behaviours (Hawgood et al 2021).
Trauma-informed care should be considered a standard precaution for all health professionals.
A lack of trauma awareness may result in clinicians unintentionally contributing to situations that re-traumatise patients or increase distress (Classen & Clark 2017, Racine et al 2020) and may affect a patient’s willingness to engage in future healthcare (Classen & Clark 2017, Heywood et al 2024).
The good news is that many of the important skills in preventing suicide overlap with existing physiotherapy competencies, such as strong interpersonal skills, the ability to collaboratively work with people and an aptitude for personal development and insight (Hawgood et al 2021, McGrath et al 2020).
Gaps in physiotherapy-specific suicide prevention training exist and could be addressed through further research and enquiry.
>> For anyone who is experiencing suicidal thoughts and behaviours or has a loved one experiencing suicidal thoughts and behaviours or has been bereaved by suicide, we ask that you reach out to someone—you are not alone and you do not have to do it alone.
>> Help is available: Lifeline chat 13 11 14, text 0477 13 11 14; Suicide Call Back Service 1300 659 467.
>> Ellen Lake APAM is a clinical physiotherapist and registered counsellor and psychotherapist. Ellen works in private practice with people who present with physical and mental health comorbidity. She is the chair of the APA Mental Health national group and has a special interest in practitioner self-care and wellbeing.
>> Ryan McGrath APAM is a clinician, educator and researcher with the University of Melbourne. Ryan’s honours and doctoral research focused on investigating physiotherapists’ practices and experiences with clients experiencing psychological and suicidal distress. He is a member of the APA Mental Health national group.
>> Sophie Shephard MACP is a physiotherapist and PhD candidate. Sophie’s research interests include psychologically informed practice and suicide prevention and novel opportunities to improve pain care and research translation through interprofessional collaboration. She is an APA Pain Physiotherapist and a member of the APA Pain national group.
Quick links:
Course of interest:
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





