
Mount Isa healthcare takes a leap forward

A pioneering telehealth clinic in regional Queensland is providing physiotherapy expertise to non- urgent patients on the orthopaedic waiting list, connecting them with care like never before.
From the moment he set foot in the entrance of Mount Isa Hospital in north-west Queensland, Stuart McCaskill had a feeling
of familiarity.
The small-town, country-hospital vibe at Mount Isa was the same as the one the British-born and trained physiotherapist experienced when he first arrived at Brisbane’s Queen Elizabeth II Jubilee Hospital (QEII) back in 2004.
And that rustic hospital ambience is something Stuart finds very comforting.
Stuart made the 1825-kilometre journey from Brisbane to Mount Isa in early 2024 for a two-day orientation and to meet the allied health team before both sites embarked on a unique partnership aimed at alleviating growing pressure on the regional hospital’s orthopaedic waiting list for category 3 patients.
Stuart, a clinical lead physiotherapist in the musculoskeletal management clinic at QEII, was visiting Mount Isa as a prelude to sharing his expertise with patients via telehealth from Brisbane, while senior physiotherapist Mackenzie Bagley and the remainder of the Mount Isa physiotherapy team would serve as Stuart’s hands and would help patients navigate the telehealth appointment.
Before beginning the new telehealth clinic at their respective locations, however, Stuart and the Mount Isa physiotherapy team
met in person at Mount Isa Hospital.
Stuart travelled to Queensland’s Gulf Country region to talk the physiotherapy team there through the new clinic, which started on
1 February this year.
Six months earlier, the consultation and advocacy process had begun to start the weekly clinic, which was the brainchild of QEII’s Director of Medical Services and previous director of orthopaedic surgery, Dr Christopher Bell.
The pilot program, recently extended for another 12 months, allows regional outpatients to connect virtually with orthopaedic and allied health specialists at QEII.
It aims to fill the gap in specialist availability in the region and is based on a model similar to QEII’s successful musculoskeletal management clinic.
That clinic saw a large number of non-urgent category 3 patients—more than 60 per cent—come off the waiting list altogether and it is hoped that this result will now be replicated in Mount Isa.
For Stuart, the trip to Mount Isa was quite an eye-opener. Despite the hospital’s familiar feel, patient stories in Mount Isa differed vastly from those of patients in Brisbane.
‘A typical patient with knee osteoarthritis in Brisbane might be concerned that they can’t walk to the shops.
'Whereas we had a patient from Normanton [490 kilometres north of Mount Isa] whose concern was that he couldn’t evade crocodiles quickly enough while he was out fishing,’ Stuart says.
‘Then we had an Indigenous man who had injured his shoulder hunting turtles and he couldn’t pull turtles into his tinnie anymore.
'That’s something you definitely don’t come across in Brisbane.’
Mount Isa Hospital is the main referral centre within the North West Hospital and Health Service.
It covers a vast geographical area and includes ambulatory, sub-ambulatory and inpatient services as well as outreach patient services.
While the hospital is serviced by an orthopaedic surgeon who travels to Mount Isa once a month, non-urgent category 3 orthopaedic patients are a lower priority.
However, since the opening of the telehealth clinic, the team has seen more than 50 patients.
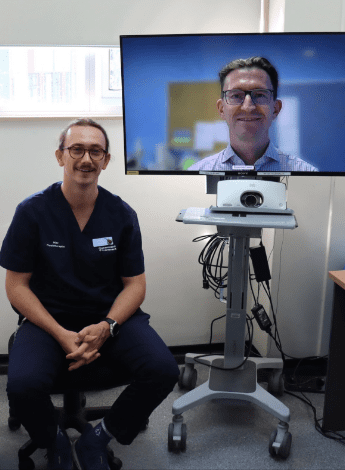
Mackenzie Bagley chats to Stuart McCaskill on a telehealth call from Brisbane.
The majority were referred on to the conservative management team, which includes physiotherapists, a dietitian, a pharmacist and a psychologist.
The telehealth clinic operates every Thursday and Stuart and a Mount Isa physiotherapist see four new patients a day in one-hour appointments, plus have two 30-minute review appointments.
Some patients travel vast distances to get to Mount Isa; one patient, who had been on the waiting list since 2021, was on holiday in Cairns when she got her appointment and she drove the 14-hour round trip from Cairns to Mount Isa to see the team.
Another group of patients was flown to Mount Isa from Mornington Island and Normanton, with some travelling by helicopter for part of the journey due to heavy flooding and road closures in the region.
The challenges of working in far-flung rural and regional healthcare settings are familiar territory for physiotherapist Mackenzie.
His first physiotherapy job after graduating from James Cook University in Townsville in 2021 was on rotation at Townsville University Hospital.
He has also worked at Brighton Rehabilitation in Brisbane as well as working as a rotational physiotherapist at Sunshine Coast University Hospital.
But what brought him to Mount Isa was a job opening and his emergency doctor partner, who had undertaken her placement at Mount Isa Hospital during her degree—and loved it.
‘She really enjoyed the remoteness of this area. Then, surprisingly, a job came up for me and when she came home I said, “We’re moving to Mount Isa.”
'I got the job as a senior rural generalist physio out here,’ Mackenzie says.
‘Our allied health clinical lead, Hannah Russell, at Mount Isa Hospital had already completed the groundwork in terms of a partnership with QEII and I saw this as an opportunity to upskill myself and to upskill in the area of musculoskeletal and orthopaedic screening service as well.’
Mackenzie says that due to the vast area serviced by the hospital, many patients live three to five hours away, often in very
remote communities, which presents some geographical challenges.
Chronic illness, diabetes-related injuries, osteoarthritis of the joints and cardiac and respiratory chronic diseases are prevalent among the population in Mount Isa City and surrounds.
‘We also live in a rural and remote town and that comes with a lot of trauma and a lot of workplace injuries and accidents.
'For example, the significant labour force out here is the hospital staff, the miners, the ringers and station workers, and the teachers as well as other Queensland Government employees such as emergency services personnel,’ Mackenzie says.
‘So we see a lot of patients who live remotely. Anything presents to the emergency department.
'One day it might be a patient with trauma-related injuries such as a conservatively managed fractured back, pelvis and/or lower limbs or patients requiring vestibular assessments, and other days it might be acute on chronic shoulder pain with history of a rotator cuff injury—anything and everything comes through Mount Isa.
'It’s a very good role in the sense of upskilling yourself, including your confidence as a clinician.’
Mackenzie, who says he benefits enormously from working with Stuart, notes that the clinic has already made a big difference to many patients’ lives.
‘We’re focusing on category 3 Mount Isa patients on the orthopaedic list, so they’ve been waiting for quite a while.
'You can imagine that some patients are very excited and very happy that they’re finally getting their issue looked at and reviewed.
'We’ve had a lot of patients who have never really had their condition explained to them.
‘Stuart is able to look at people’s X-rays with them, provide that education that they haven’t been given and say “You may not need surgery after all; let’s try some physiotherapy instead.”
'Nine times out of 10 this is received very well and people are relieved not to have surgery.
'Not only is this a significant benefit to the patients, but it is also a great opportunity for the Mount Isa physiotherapy team to upskill in this area, improving their knowledge and skills when treating their own patients.
'We have just created a rotational model for our junior physiotherapist out here, and this clinic is involved in the generalist/telehealth rotation; it’s a great way for our junior clinicians to learn and grow.’
Telehealth is a significant part of the health service delivery at Mount Isa Hospital, not only within physiotherapy but also among the wider allied health services.
As such, the allied health department had received training and upskilling in the use of telehealth before the virtual clinic started in February.
Stuart, too, had previous exposure to telehealth services at QEII during the COVID-19 pandemic.
Although not a fan of telehealth in the early days of the pandemic, Stuart realised its enormous potential for application in rural and remote healthcare settings and has been proud to work on and help create the virtual clinic now in operation at Mount Isa.
‘I’ve been pleasantly surprised by how successful this clinic has been,’ Stuart says.
‘When we do it, it’s like I’m there in the room. Apart from not being able to touch the patient, it’s just like I’m there. It doesn’t feel remote at all.’
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.





