Rehab with robots
Researchers in the NeuroRehabilitation and Robotics Laboratory at Edith Cowan University are putting robotics to work to assist patients with their rehabilitation.
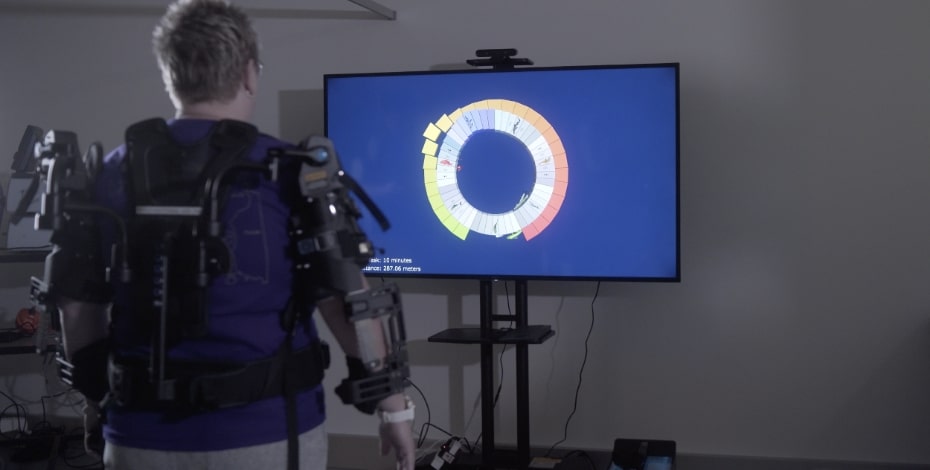
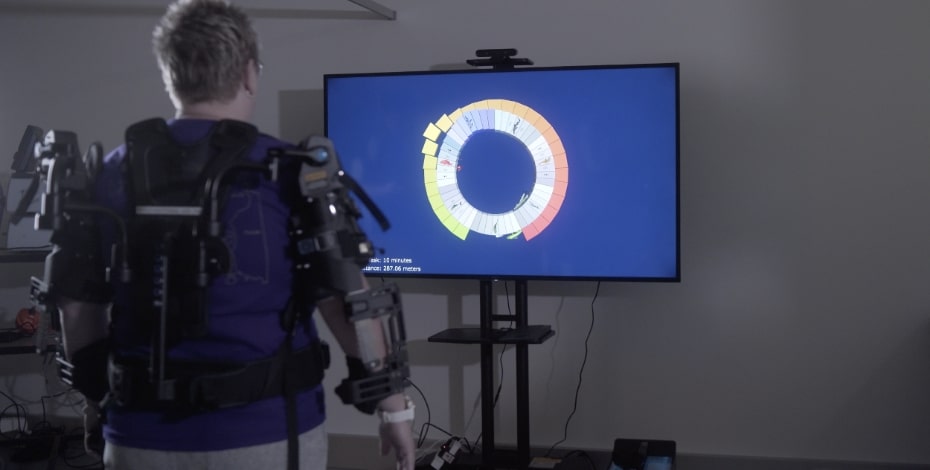
A multidisciplinary research group based at Edith Cowan University (ECU) in Perth is looking at the use of robotic technology to take on some of the rehabilitation load in patients with neurological conditions, allowing patients to do longer sessions of therapy by keeping them actively engaged and providing assistance and support as required.
‘We predominantly work with adult humans who have acute neurological conditions, so we’re talking about stroke and spinal cord injury, and some degenerative diseases, and our research is mostly to do with the motor systems,’ says physiotherapist and neurorehabilitation researcher Professor Dylan Edwards, director of ECU’s NeuroRehabilitation and Robotics Laboratory and of the Moss Rehabilitation Research Institute in Philadelphia, USA.
The NeuroRehabilitation and Robotics Laboratory is investigating the use of available technologies to improve movement and motor function by taking advantage of the brain’s capacity to rewire itself after a neurological injury.
Rehabilitation already draws on the brain’s plasticity, but the process of retraining the brain can require a lot of intensive physiotherapy, occupational therapy and other assistance.
The robotic assistive devices help the patient to stay in position and remain engaged in doing the exercise, allowing them to do a higher number of repetitions than in a conventional therapy session.
The aim, says Dylan, is to use the technology to make someone more independent after completing rehabilitation, not dependent on the robotic device.
‘It’s still good old-fashioned physiotherapy, but it’s the behavioural training component that we really focus on.
'We use the technology to help deliver the required dose of rehab because we know that simply doing something 10 times in a physio session is not enough when we’re talking about brain plasticity and rewiring, regaining strength and function and reducing impairment,’ he says.
The laboratory uses a number of different technologies in its work with patients, says research fellow Dr Onno van der Groen.
These include gamified environments tailored for repetition—for example, an underwater environment in which a patient supported by an exoskeleton uses their arms to control the movement of a dolphin.
The technology allows them to do high-dose, high-repetition studies where patients complete a 70-minute-long program of therapy six times a week for six to eight weeks.
So far, the technology has been used with patients who are hemiparetic—they have paralysis down one side of the body, a common occurrence in survivors of stroke—to exercise the upper extremities, the hands and arms.

Professor Dylan Edwards leads the NeuroRehabilitation and Robotics Laboratory at Edith Cowan University.
While the initial studies involved patients who had moved to outpatient rehabilitation, the team is now interested in working with inpatients at an earlier stage of rehabilitation, soon after the injury when the brain has increased plasticity.
‘It’s a better time for recovery and it’s easier to get the intensity [of repetitions] up there,’ Dylan says.
The ability to use the equipment in a home setting is also attractive.
A clinical study in which the lab is involved has shown that repetitive, game-based therapy—including target practice, turning knobs and dexterity exercises as well as education about stroke risk factors and so on—is as effective when done at home as it is when done in the clinic.
‘We’re pretty excited because, while this type of therapy has limitations, it changed their Modified Rankin Score [an important outcome measure for stroke studies] by a point, which is meaningful in these trials.
'It makes the patient more independent,’ Dylan says.
While the robotic devices assist patients with movement and support as they do their exercises, they do have less value for patients who can’t move their limbs at all.
In these patients, however, some of the devices can be used as an assessment tool to look at the passive joint range, proprioception and more.
The ECU team is also investigating the use of non-invasive brain stimulation techniques to increase brain plasticity and to improve voluntary movement and motor function, such as transcranial direct current stimulation and transcranial magnetic stimulation in combination with repetitive motion activities.
‘The evidence isn’t there yet for non-invasive brain stimulation.
'It’s a little bit frustrating; it looks like it works in some patients but we still don’t have a really robust effect across all patients.
'If this works, it would be a tool that a therapist could incorporate into their daily practice,’ says Dylan.
‘These technologies have a place where a lot of repetitions are required to rebuild strength and movement patterns that can then be adapted into function by the therapist.
'It’s a pretty exciting time, actually, because the technology is becoming more available and at a cheaper price.
'It’s important for therapists to understand the limitations of these technologies—just like other gadgets, they are important tools for the right kind of patient when done the right way, but they are not a substitute for physical therapy.’

Dr Onno van der Groen is a research fellow in the Laboratory.
Transcranial magnetic stimulation can also be used to evaluate the status of the motor system—that is, whether the corticospinal tract is still intact—and this information could be used to develop mathematical models predicting how well a patient might respond to a specific therapy, says Onno.
A neuro-navigation system, like a GPS for the brain, is used to optimise the precision of brain stimulation.
‘We are trying to capture everything—the clinician’s evaluation plus the neuroimaging showing exactly where the lesion is in the brain and other features, including demographics such as their age and gender.
'You can then use a data-driven mathematical approach where the AI takes this information and shows that the most important feature was, perhaps, your clinical assessment of some impairment score, but their age was important and maybe where the lesion is located was also important.
'And it can pull out the features that will predict whether patients are going to respond to a therapy and what their predicted recovery is,’ Dylan says.
Dylan expects that eventually clinicians will be able to access a prescription algorithm that helps them decide whether a particular therapy is likely to help a patient, based on the information collected.
APA Neurological Physiotherapist Jimena (Mena) Garcia-Vega MACP, senior physiotherapist on the neurosurgical wards at Sir Charles Gairdner Hospital in Perth, is collaborating with the laboratory on several studies.
Mena’s main study, in collaboration with Professor Taiza Edwards and colleagues at the University of Sao Paulo in Brazil, is looking at the presence of lateropulsion (informally known as Pusher syndrome) in patients after brain tumour removal.
Lateropulsion includes an array of motor, sensory, perceptual and cognitive impairments resulting from damage to specific areas of the brain, causing abnormal body alignment, verticality and motion.
It often presents after stroke, but is also seen after a traumatic brain injury or in patients with brain tumours (pre and post-surgery).

Physiotherapist Mena Garcia-Vega is collaborating with the Laboratory.
Mena’s study considers a variety of available assessments in patients who have had brain tumours removed to identify motor, sensory and perceptual impairments in relation to specific areas of the brain affected.
Imaging analysis and brain mapping technology were used to correlate the severity of impairment with affected brain areas and to inform predicted functional recovery in this specific cohort.
While most of the lab’s studies involve neurological injury, its researchers are also working with ECU’s Systematic Profiling in Neurological Conditions research program, funded by the Multiple Sclerosis Society of Western Australia, which aims to systematically profile people living with neurological conditions, including Parkinson’s disease, multiple sclerosis and dementia, in addition to acquired injuries.
‘We use some of our robotics to look at movement kinematics, while other people on the project look at cognition or speech, and people come back every year for us to track the progress of their disease and how it changes over multiple years.
'We also have a few interventions that tie in with this observational study.
'So we can, for example, offer people who are showing motor deficits due to stroke an intervention to target these impairments using our technologies,’ says Onno.
Dylan and his team work closely with a number of companies to explore the use of their technologies in rehabilitation settings and then adapt them.
It’s a win-win system for both parties as the research team can work with the company to tweak the robotic systems to better suit the rehabilitation protocols, while the company gets data that supports the evaluation and approval process required by the Therapeutic Goods Administration before a device can be marketed in Australia.
Both the assessments and the interventions they hope to develop from their research are likely to combine multiple devices to achieve the desired result, rather than just using one device.
For example, a motor intervention using an assistive robot could be combined with a non-invasive brain stimulation device to increase the plasticity of the brain during the rehabilitation sessions, Dylan suggests.
Ultimately, the lab’s research is focused on improving rehabilitation for patients with neurological injuries and conditions.
‘It’s about trying to improve people’s lives.
'If we can help a patient get some of their motor function back, they can have a better quality of life,’ Dylan says.
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





