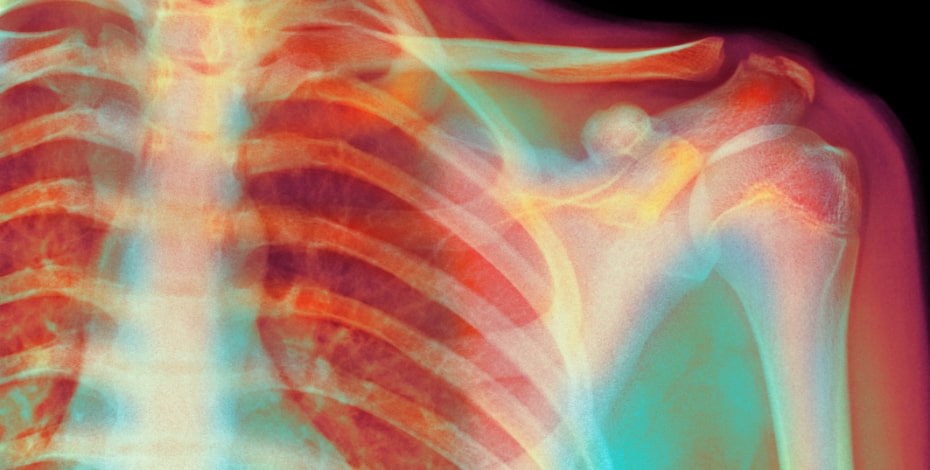
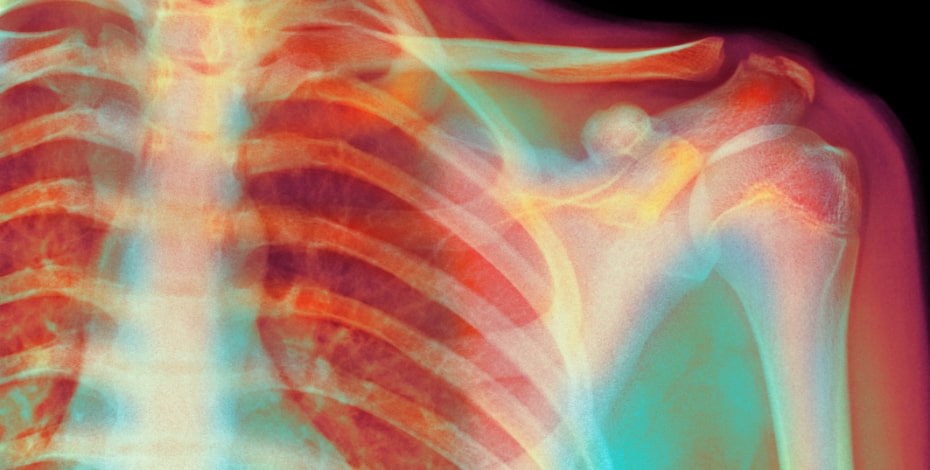
Subacromial impingement: is it time we finally abandoned the term?
The past 15 years have seen tremendous change in the musculoskeletal (MSK) medicine landscape. At the centre of this has been a reconceptualisation of how we understand various common non-traumatic clinical conditions, including non-specific low back pain, osteoarthritis and tendinopathy, to name a few.
This deeper understanding has involved an appreciation of the true multidimensional nature of many MSK pain presentations (O’Sullivan 2018). This progress has been at the expense of the hitherto dominant biomedical model where pain is thought to arise secondary to frank pathology in the peripheral tissue, in a classic dualist manner.
Don’t get me wrong: the biomedical model has fostered many important advances in medicine and has been instrumental in improving quality and length of life for people far and wide (Borrell-Carrio et al 2004).
The advent of antibiotics, vaccinations, and many surgical procedures has saved an untold amount of lives worldwide and it is not my intent to diminish this.
However, for many MSK pain presentations, and especially persistent pain, the biomedical model in isolation can’t adequately cope with the complexities of pain and tends to reduce complex, non-linear organisms (human beings) to mechanical bits and parts.
To offset the limitations of the biomedical model, the biopsychosocial (BPS) model was suggested as a more holistic approach to medicine (Engel 1977) and pain (Gatchel et al 2007).
While the BPS model was coined over 40 years ago, we have only recently started to apply it to common clinical MSK conditions with any gusto. I contend the ubiquitous shoulder condition, subacromial impingement (SAI), when viewed through the lens of the BPS model, becomes an untenable term and one we should stop espousing urgently.
The term SAI can be traced back to Dr Charles Neer in 1972 who stated ‘95 per cent of rotator cuff tears are initiated by impingement wear’ of the rotator cuff and bursa against the overlying acromion (Neer 1983), based solely on anecdotal observation.
To treat this ‘impingement lesion’, Neer popularised the anterior acromioplasty surgical procedure (Neer 1983), now colloquially referred to as subacromial decompression (SAD).
This procedure became the gold standard intervention to manage SAI and led to an exponential increase in its application after the advent of arthroscopic surgical techniques (Judge 2014). SAI was subsequently enthusiastically accepted as the primary driver of shoulder pain and pathology of the rotator cuff, and went virtually unchallenged for the better part of half a century.
By the late 2000s some rumblings among the physiotherapy community on the nebulous concept of SAI began to emerge, culminating in a seminal narrative review by Jeremy Lewis, PhD (Lewis 2011), which challenged the accepted pathogenesis, diagnosis and management of SAI.
At the heart of this review (now nearly 10 years ago) was the demonstration of consistently equivalent outcomes of SAD surgery compared to exercise therapy to manage symptomatic SAI.
This finding has been repeatedly validated during the intervening 10 years with a number of high-quality reviews and randomised controlled trials reporting no clear benefit of SAD versus exercise therapy (Lahdeoja et al 2019) or placebo (Karjalainenet al 2019, Paavola et al 2018).
This raises an awkward question: if SAD surgery is not superior to placebo or exercise therapy for pain and function, or leads to reduced incidence of rotator cuff tears (Kolk et al 2017), does the ‘impingement’ component of the condition, which is fundamental to the philosophy of SAI, become obsolete?
Proponents of evidence-based practice would argue yes, as the ‘impinging lesion’ remains in situ but symptoms have improved markedly, casting doubt on the role and relevance of impingement (Beard et al 2018).
It is becoming clearer that impingement need not be surgically reduced to appreciably improve a person’s pain, function and quality of life.
In fact, recent research has shown the biggest predictors of physiotherapy outcomes for people with shoulder pain are not mechanical features at all, but patient expectations and self-efficacy (Chester et al 2019, Dunn et al 2016).
Evidence is also starting to accumulate suggesting a relationship between rotator cuff-related shoulder pain and metabolic syndrome, which highlights a potential systemic physiological influence in the pathogenesis of SAI (Burne et al 2019).
These findings are unsurprising given what we are now beginning to understand about the role of beliefs, expectations, and lifestyle factors in the pain experience (Tabor et al 2017, Nijs et al 2019) and the more disparate the relationship between pain and the state of the tissues becomes, the longer the duration of pain (Wall 1979).
The term subacromial impingement may not only be tenuous from a pathogenesis perspective, but perversely, it may act as a barrier to recovery.
In a recent qualitative study, Cuff & Littlewood (2018) interviewed people who had been diagnosed with SAI about what the diagnosis meant to them, and the responses were dire from a physiotherapy perspective.
Answers included: ‘If there is a physical lump or something there, all the physiotherapy in the world isn’t going to resolve that if that doesn’t disappear. He said it was quite likely that I might well need some keyhole surgery’; and ‘I can’t imagine how any amount of physio is going to shift this piece of bone in my shoulder’.
It is little wonder that a person interprets their diagnosis in this way, as this is what the term inherently suggests. Given how crucial patient expectations are to recovery, are we (physiotherapists) setting ourselves up for failure?
To counter this, there has been a push to rebrand SAI as rotator cuff-related shoulder pain (RCRSP) (Lewis 2016) or subacromial shoulder pain (SSP). These umbrella terms reflect the non-specific nature of the condition, similar to non-specific low back pain, which has mostly been integrated into general practice despite initial resistance.
The rebranding reflects the true multidimensional nature of the condition with physical, psychological, genetic, social, lifestyle, and physiological underpinnings (Maestroni et al 2020) but also positions physiotherapy and exercise as the primary intervention.
The ‘physical’ aspect of SSP still has an important influence on pain and function of the shoulder, no question; it just may not be as strong a relationship as we once thought and there is no strong evidence it is more important than the aforementioned factors.
While there have been rumblings and murmurings about the name ‘SAI’ for the better part of a decade, I propose it is now time to actively reject it as a term of any accuracy or utility and strongly recommend we promote the use of RCRSP or SSP to reflect the multidimensional nature of the condition.
This will not only serve physiotherapy well, but more importantly, our patients.
>> Email inmotion@australian.physio for references.
Jared Powell, APAM, is a senior physiotherapist at Physio Place in Tweed Heads, NSW, and is currently completing his PhD in rotator cuff-related shoulder pain under Jeremy Lewis, PhD, at Bond University, where he is also a visiting lecturer and tutor. Jared teaches shoulder workshops in Australia and overseas.
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





