
Switching on the lightbulb to see hypermobility disorders

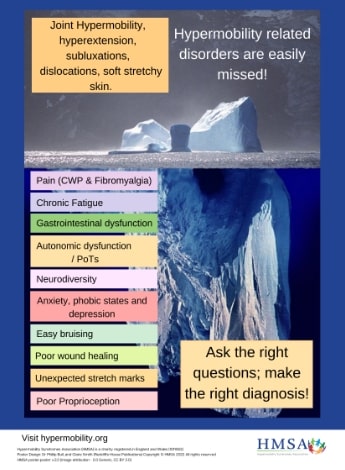
A collection of physiotherapists with an interest in treating adults and children with hypermobility disorders hopes to raise awareness of the conditions. Juliet Hall, Sharon Hennessey, Pauline Slater, Clare Adams, Nicole Frost and Katie Cleary explain why screening of current clients for hypermobility spectrum disorder is important.
Hypermobile joints occur in approximately three to 25 per cent of the population.
They certainly aren’t always a bad thing.
Asymptomatic hypermobility can be a significant advantage in a number of sports, but there are many people with connective tissue disorders whose daily lives are moderately or severely affected.
Physiotherapists may already be familiar with the Beighton score, but here is a refresher:
The scale includes the ability to touch palms flat to floor with knees straight (one point), elbow extension >10 degrees (one point for each side), knee extension >10 degrees (one point for each side), the ability to touch thumb to forearm (one point for each side) and fifth finger metacarpophalangeal joint extension >90 degrees (one point for each side) with the option to place the finger on the table and measure the angle with the hand.
A positive Beighton score for adults is five out of nine possible points; for adults over 50 it is four out of nine and for children it is six out of nine.
An alternate screen by Hakim and Grahame from 2003 (the Five-Part Questionnaire for Hypermobility) could be a great addition to your pre-assessment questionnaire.
Ask your clients the following questions:
- Can you now (or could you ever) place your hands flat on the floor without bending your knees?
- Can you now (or could you ever) bend your thumb to touch your forearm?
- As a child, did you amuse your friends by contorting your body into strange shapes or could you do the splits?
- As a child or teenager, did your shoulder or kneecap dislocate on more than one occasion?
- Do you consider yourself double-jointed?
A score greater than two out of five is considered positive for hypermobility.

Reproduced with permission of the Hypermobility Syndromes Association.
Establishing whether a client is/was hypermobile (visible joint signs of hypermobility can lessen with age due to injury and effects of ageing) is only the first step.
The second step in the diagnosis of hypermobility spectrum disorder (HSD) is finding secondary musculoskeletal manifestations (eg, joint instability, chronic pain or disturbed proprioception) in the absence of other explanations (eg, rheumatic conditions).
HSD has superseded the previous term of joint hypermobility syndrome and has the subcategories of generalised, historical and local or peripheral.
A diagnosis of hypermobile Ehlers-Danlos syndrome (hEDS) is made by a medical specialist, most commonly a rheumatologist or geneticist.
Specific criteria now distinguish hEDS (previously known as EDS type 3) from HSD, including family inheritance and other common features such as body morphology and skin.
Neither a diagnosis of HSD nor a diagnosis of hEDS indicates a greater degree of severity of symptoms than the other does and they are both considered connective tissue disorders.
‘Diagnosing a child with HSD or hypermobility often involves a subsequent diagnosis for their parent of hypermobility, a condition that has often affected them for their whole life that they never knew about,’ says physiotherapist Katie Cleary APAM.
What is the point of diagnosis?
In a recently published masterclass in hypermobility, internationally renowned physiotherapist Jane Simmonds says, ‘Early recognition and treatment of hypermobility-related disorders is key to effective management.’
Queensland physiotherapist Sharon Hennessey APAM agrees, saying that just because hypermobility-related disorders are common, it does not mean they should be ignored.
‘Obesity is common.
'Depression is common.
'But clients are offered appropriate medical care for these issues.
'Hypermobility should be given the same respect,’ Sharon says.
‘It isn’t simply chronic pain that is experienced by these clients.
'There are additional frequent acute and subacute local tissue issues that are still healing, often wrapped up in a package of sensory sensitisation.’
Earlier in her career, Sharon had a 17-year-old client (BB) who was referred for lateral hip pain.
On the first appointment, the client seemed a little distant and laughed when talking about her pain, saying, ‘I am just weird.’
BB had seen multiple physiotherapists throughout her life and was often discharged due to failure to progress. BB was very intelligent, was in her first term of studying occupational therapy and was struggling with her workload, reportedly suffering fatigue, dizziness and pain flare-ups.
Reproduced with permission of the Hypermobility Syndromes Association.
On deeper probing, Sharon found that BB was falling weekly due to her ankles giving way or sometimes due to blackouts, that she had fractured her wrist and fibula in the past six months and that she had not been able to complete the program at an adolescent pain clinic and had complex regional pain syndrome in her elbow from a previous injury while at high school.
Sharon says BB complained of gut pain and had difficulty maintaining her weight.
BB’s Beighton score was nine out of nine and her Five-Part Questionnaire for Hypermobility score was three out of five.
Sharon put together her issues and recognised her HSD.
Eight weeks later, despite doing her exercises, BB did not make progress with her control of one leg balance and she did not report any reduction in pain levels.
‘This is not unusual with clients with hypermobility, so treatment continued and she made significant gains but over a much longer period than would have been expected with a regular client.
'Letters were sent to her GP as well as a session with her family to explain HSD,’ Sharon says.
‘The multidisciplinary team became involved, including psychology, dietetics, podiatry, cardiology and genetics (for hEDS assessment) as well as her attending a weekly clinical Pilates class.
‘BB’s progress often hit roadblocks, including an ankle stabilisation (with complex regional pain syndrome complication), her passing out in the clinic from malnutrition (due to gastroparesis) and the insertion of a percutaneous endoscopic gastrostomy for supplemental feeds.
'But the rewards of working with BB long-term have been enormous, including seeing her self-worth build when she got her official hEDS diagnosis and seeing her graduate from university and successfully work full-time as an occupational therapist.’
Private practitioner Pauline Slater APAM says, ‘When receiving a diagnosis after a difficult journey, patients finally have an answer, leading them to a place from which the healing process can begin.’
She reported a 36-year-old mother of three children, who all have HSD, saying, ‘Being misdiagnosed for nearly 15 years by multiple health professionals resulted in me being in pain since I was 14 years old.
'I feel angry about what’s happened to me.
'At many points in time I thought it was all in my head, but it turns out that it’s my body.
'I have hEDS and it impacts every aspect of my life.
'The great news now is that I can help my kids.’
The average time between onset of symptoms and diagnosis with a hypermobility disorder is 10 years.
Between 80 and 90 per cent of hEDS and HSD clients first present with pain.
Pauline says the group would love the time between onset of symptoms and diagnosis to be shorter and she encourages all physiotherapists to be a part of the change to make that happen.
What are the common roadblocks for rehabilitation of hypermobility?
The widespread issues associated with HSD/hEDS often result in poor outcomes from mainstream rehabilitation programs.
This can be affected by underlying issues including increased healing time, neurological dysfunction (small fibre neuropathy, dysautonomia and proprioception deficits), dizziness, fatigue, anxiety, neurodiversity and impaired nutrition.
As the building block of connective tissue, collagen is distributed throughout the body, so manifestations of HSD/hEDS can be present, to varying degrees, in virtually every body system.
Making a difference for your new-found symptomatic hypermobile client
Physiotherapist Nicole Frost APAM says, ‘With an understanding of the widespread effects of hEDS/HSD on affected clients, our physio colleagues can shift the experience of treating these clients from frustrating to rewarding, while simultaneously moving the client’s experience from demoralising to positively life-changing.’
Clare Adams APAM agrees, saying, ‘It’s about turning survive into thrive.’
The group advises that physiotherapists could:
- screen every client for hypermobility
- listen and believe their clients’ lived experience without judgement
- check for systemic manifestations of connective tissue issues
- look at the entire musculoskeletal picture, not just focus on the specific presenting problem
- involve and educate their multidisciplinary team about HSD.
Making the connection
The network of physiotherapists in this article is passionate about advocacy for clients with hypermobility disorders.
The group came about through frustration with how poorly hypermobility disorders are understood and managed, in both the physiotherapy and medical communities.
Physiotherapist Juliet Hall says she first started to look for hypermobility after a conversation with a potential employee.
Screening her next two exercise classes, Juliet found that seven out of eight of the clients were hypermobile.
‘After more than 20 years as a physio, I was amazed that issues related to hypermobility had flown under my radar for so long.
'I joined the free EDS ECHO program to learn more.
'I connected with a wonderful network of therapists and felt inspired to raise awareness about hypermobility disorders.
‘As well as helping clients with the significant functional issues that result from their connective tissue disorders, I am now equipped with skills to better manage my existing clientele.
'My team now screens for hypermobility routinely, as a positive result impacts our understanding of a client’s biomechanics and alerts us to the need to look for other potential comorbidities,’ she says.
EDS ECHO is a series of programs for healthcare professionals across all disciplines who want to improve their ability to care for people with Ehlers-Danlos syndromes, hypermobility spectrum disorders and associated symptoms and conditions.
>> Juliet Hall APAM is the founder and director of Bodyfit Physio in Northcote, Melbourne, which provides a variety of physiotherapy services for adults and children. Her interest in hypermobility springs from discovering a need for quality management and advocacy for this group.
>> Sharon Hennessey APAM is the principal physiotherapist and founder of Not Just Bendy Hypermobility Services—a private musculoskeletal practice in Brisbane for those with complex hypermobility and Ehlers-Danlos syndrome (EDS). Sharon has a passion for treating hypermobility. She has presented to APA special interest groups and to the EDS ECHO program and also presented a poster at the EDS ECHO Summit in 2020.
>> Pauline Slater APAM is the principal physiotherapist and founder of Bendy Bodies Hypermobility Physiotherapy in Adelaide. Pauline assists clients of all ages with learning difficulties, neuroeducational disorders and complex musculoskeletal, hypermobility and pain conditions. She is pursuing a PhD in awareness and education of the medical and allied health professions regarding HSD and EDS.
>> Clare Adams, APAM, is a senior physiotherapist with Queensland Health working at Redcliffe Hospital covering paediatric and adult specialist orthopaedic and outpatient clinics. Clare has a specific interest in HSD, and paediatric and adult pelvic health.
>> Nicole Frost APAM has a keen interest in clinical research and is a National Health and Medical Research Council grant recipient. Nicole is the founder and director of Flex-Ability Physio, a practice focused on the management of issues related to HSD. She has attended the Paediatrics and the Allied Health Professionals (AHP) EDS ECHO programs and guest presented on the AHP program. She is a member of an international committee on cervical pathology related to HSD.
>> Katie Cleary APAM is the Director of Ocean Kids Physiotherapy in Melbourne. Katie enjoys helping children living with HSD and EDS and she has completed extensive professional development in paediatric hypermobility management. She is a member of the paediatric working group with The International Consortium on Ehlers-Danlos Syndromes and Hypermobility Spectrum Disorders.
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





