Have you read the latest research?
JOURNAL OF PHYSIOTHERAPY With the next issue just around the corner, there’s still plenty of quality research from the January issue to tide you over. Here are two examples.
RESISTANCE TRAINING IN ADOLESCENT IDIOPATHIC SCOLIOSIS
The results of this trial indicate that adolescents with idiopathic scoliosis respond more positively to aerobic and resistance training combined than to aerobic training only. Q&A with Dr Vera Alves.
What is adolescent idiopathic scoliosis (AIS)?
AIS is a lateral curvature in the spine that has its onset usually after 10 years of age. The curvature shows rapid progression during growth and it is often accompanied by a variable degree of rotation of the spinal column. The spinal curvature can be measured by
X-ray, where specialists calculate ‘the Cobb angle’: the higher this value, the more severe the spinal curvature is. This ‘torsion’ of the spine represents more than just issues of aesthetics: adolescents with AIS have other clinical problems that are due to this deformity.
What symptoms does it cause?
Because of the torsion in the rib cage caused by the spinal deformity, a person with AIS may present with shortness of breath, because the lungs don’t have space to get full of air, and because the muscles that move the rib cage and help us breathe are weak too. But even if the patient with AIS is asymptomatic, respiratory function tests may reveal impairment of breathing. In addition to ventilatory restriction, the muscle weakness that lead to respiratory dysfunction also cause exercise limitation, thereby changing the physiological responses to activities of daily living and resulting in functional disability in many cases.
What do we already know about the effects of exercise in this clinical population?
Adolescents with a Cobb angle of 45 degrees or more are considered to have severe AIS, and there is an indication for surgery in these cases because of the associated dysfunction. The literature shows that a program of standardised activity for these patients with severe deformities significantly improves cardiorespiratory and musculoskeletal conditioning. However, the most beneficial type of exercise remains unclear.
How did you design your study to address this issue?
We conducted a randomised clinical trial involving 40 adolescents with idiopathic scoliosis and formal indication for surgical correction (spinal curvature ≥ 45 deg). All participants undertook three 60-minute training sessions per week for 12 weeks. Half were allocated to an experimental group, which performed combined aerobic and resistance training. The other half were allocated to a control group, with only aerobic training.
What did you find?
After 12 weeks of training, the group of adolescents performing the combined aerobic plus resistance training had significantly more improvements than the control group. First, they could walk more: on the 6-minute walk test, they could walk on average 22 metres more (with a 95% confidence interval, CI, from 4 to 40). Patients doing the resistance training also had the perception that they had to exert less effort to do the same exercise (this is called perceived exertion) at the end of the test (on average –1.2 points on the Borg scale, 95% CI –1.9 to –0.4). The experimental group also improved more than the control group on several respiratory measures, including FEV1 (MD 270 ml, 95% CI 30 to 510), maximal inspiratory pressure (MD 4 cmH2O, 95% CI 1 to 8) and peak expiratory flow (MD 33 l/minute, 95% CI 7 to 58).
Are those effects considered worthwhile?
If we consider each of these benefits in isolation, one might think that the effects are probably not clinically worthwhile, because they may be considered very small. However, the combined effect of all these small benefits suggests that it is worth recommending the addition of resistance exercise to the aerobic training to adolescents with idiopathic scoliosis. Because this study was small, we are following up this group of adolescents until they are operated on, to see if this slightly better fitness leads to better clinical condition after surgery. Clinicians might also consider other issues when prescribing exercise training to these adolescents; for example, a patient may prefer and be more compliant with aerobic training
Reference
Xavier VB, Avanzi O, de Carvalho BDMC, Alves VLS (2020) Combined aerobic and resistance training improves respiratory and exercise outcomes more than aerobic training in adolescents with idiopathic scoliosis: a randomised trial. Journal of Physiotherapy
>> Vera Lúcia dos Santos Alves has long-time experience conducting studies on adolescent idiopathic scoliosis in a philanthropic hospital in Brazil. She is a senior researcher and tenured teacher in physiotherapy in a medical and physiotherapy school, where she leads a team of postgraduate researchers and graduate students.
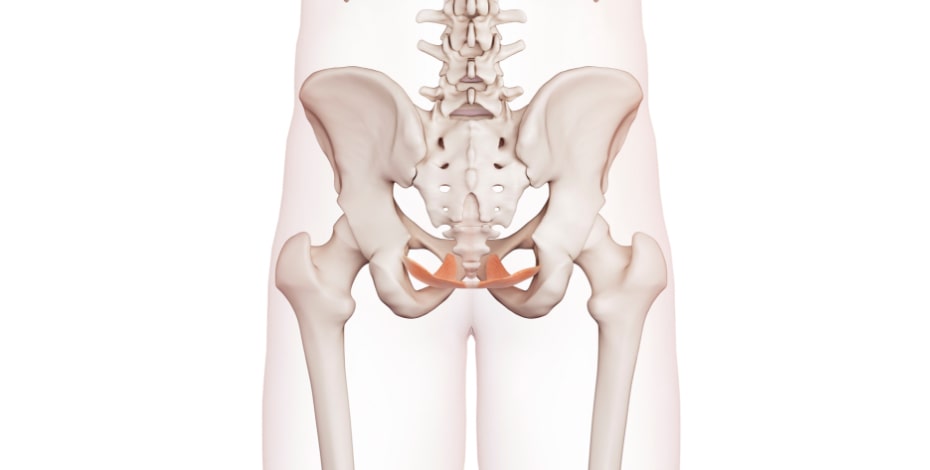
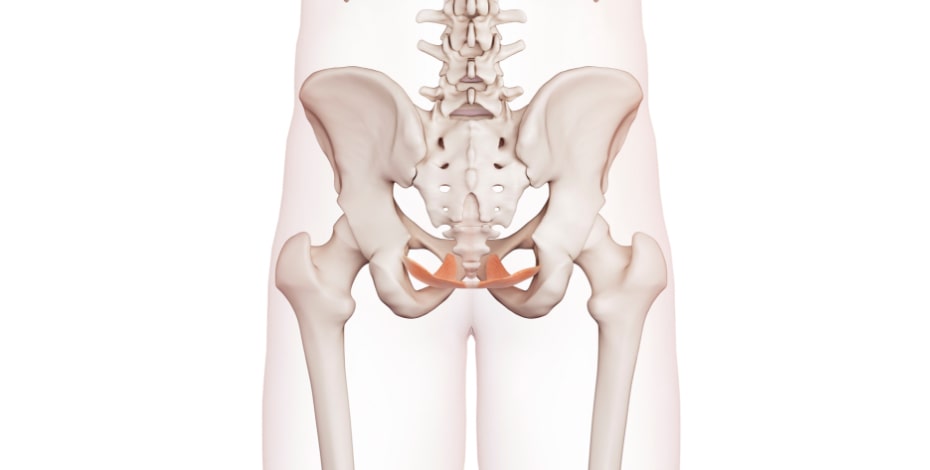
PELVIC FLOOR MUSCLE TRAINING IN PROLAPSE SURGERY
The results of this study support the existing evidence that perioperative pelvic floor muscle training does not add any worthwhile additional short-term benefit to surgery for pelvic organ prolapse symptoms. Q&A with Associate Professor Cristine Ferreira.
What is pelvic organ prolapse and how common is it?
Pelvic organ prolapse (POP) is a downward displacement of part of an organ, commonly the uterus and/or the different vaginal compartments and neighbouring organs such as the bladder, rectum or bowel (ICS/IUGA 2016). The POP-Q is a reliable and valid clinical method that measures each prolapse compartment separately (anterior, posterior and apical). After the measurements of defined anatomical points in relation to a fixed point (the hymen) are taken, the stage of the POP is classified from 0 (no prolapse is demonstrated) to 4 (complete vaginal eversion). The assessment of POP symptoms is essential as discrepancies in relation to objective findings frequently occurs. The classic and most valid symptom of POP is the sensation of a bulge in the vagina.
Comorbidities of urinary, bowel and sexual symptoms are common. The prevalence of anatomical prolapse measured with POP-Q is around 50 per cent, while the prevalence of symptoms impacting women’s quality of life usually varies between 3 and 15 per cent.
How is pelvic organ prolapse managed?
Therapeutic options for POP include surgery and conservative treatments such as insertion of a pessary or pelvic floor muscle training (PFMT). Recent systematic reviews have concluded that PFMT reduces POP symptoms and severity stage. In addition, PFMT also increases pelvic floor muscle (PFM) strength and endurance, reduces the levator hiatus area, lifts the bladder and rectal ampulla, increases PFM volume, and reduces PFM length. Surgery is effective in many, but the recurrence rate after surgery can be up to 54 per cent, varying greatly according to the surgical technique and other variables. Surgery, especially using mesh, has had complications in many women.
How did you tackle this problem with your study?
It could be assumed that the success rate of POP surgery would increase by combining surgery with PFMT delivered both before and after the surgery. Therefore, we conducted a randomised clinical trial to examine that.
Had anyone previously looked at that?
Yes, a few randomised trials had been conducted to evaluate the effect of combining POP surgery and PFMT on POP symptoms. However, recent systematic reviews concluded that there is insufficient evidence to affirm whether incorporating perioperative PFMT improves the benefit obtained from surgical repair of POP.
How was your trial set up?
Ninety-six women with an indication for POP surgery were enrolled. Half were randomised to an experimental group, which received a nine week pelvic floor muscle training protocol with four sessions before surgery and seven sessions after surgery. The remaining women were allocated to a control group, and had surgery only.
What did the results show?
There was no substantial difference in POP symptoms between the experimental and control groups at days 40 and 90 after surgery. On a scale from 1 (very much better) to 7 (very much worse), the experimental group perceived marginally greater global improvement than the control group; mean difference –0.4 (95% CI –0.8 to –0.1) at Day 90. However, the estimated effect of additional perioperative PFMT was estimated to not be beneficial enough to be considered worthwhile for any other secondary outcomes.
What would you recommend for these women then?
In women undergoing POP surgery, additional perioperative PFMT had negligibly small effects on POP symptoms, PFM strength, quality of life or sexual function. However, given the evidence that PFMT is effective in reducing POP symptoms and improves anatomical POP in POP-Q stages I, II and III, it seems essential that women with POP stage I to III are offered an evidence-based PFMT protocol as first-line treatment before surgery is considered.
Reference
Duarte TB, Bø K, Brito LGO, Bueno SM, Barcelos TMR, Bonacin MAP, Ferreira CHJ (2020) Perioperative pelvic floor muscle training did not improve outcomes in women undergoing pelvic organ prolapse surgery: a randomised trial. Journal of Physiotherapy
>> Cristine Homsi Jorge Ferreira (PT, PhD) specialises in women´s health physiotherapy and is an associate professor in the Health Sciences Department at Ribeirão Preto Medical School, University of São Paulo, Brazil. She has been a women´s health associate editor of the Brazilian Journal of Physical Therapy since 2018.
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.





