Tablet-based exercise in wrist, hand and finger injuries
Do feedback-guided exercises performed on a tablet touchscreen hasten return to work, reduce healthcare usage and improve clinical recovery more than a home exercise program prescribed on paper? Q&A with María-Dolores Cortés-Vega.
Your trial compared two different approaches to providing a home exercise program after a bone or soft tissue injury of the wrist, hand and/or fingers. What are some examples of the sorts of injuries that the study participants had?
The most frequent set of pathologies in the clinical trial were fractures of the radius, ulna, and scaphoid; fractures of one or more phalanges of the hand; and disorders of synovium, tendon and bursa.
What was the home exercise program that was prescribed on paper to the control group?
The exercise program used in the control group was the one conventionally used in most hospitals of the health systems: an exercise program on paper where a series of movements involving different functions of the hand and fingers are performed.
Some of the exercises were with a (semi-) closed fist, wrist flexion and extension; with the hand placed on a table, extension of the fingers one by one; and contact of each finger’s pad with the thumb pad.
What about the experimental group? How was their home exercise program delivered?
ReHand is an application created for rehabilitation after bone and soft tissue injuries of the wrist, hand and fingers.
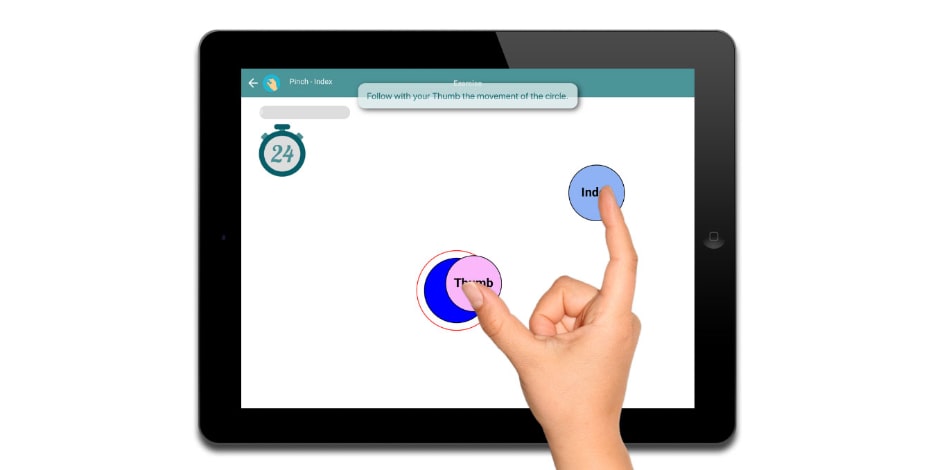
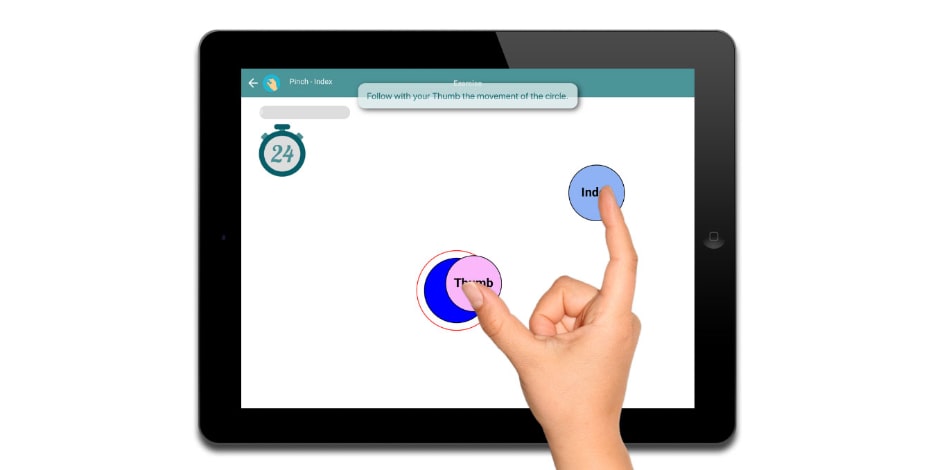
It provides monitored exercise programs guided by feedback and performed on the touchscreen of a tablet device.
But ReHand is not just an app, it comprises a treatment system for patients (ReHand app), and a web-based prescription and monitoring system for healthcare professionals.
ReHand has been developed by healthcare professionals such as physiotherapists, occupational therapists, surgeons and physiatrists, to meet the needs of patients and professionals.
What outcomes did you measure in the study?
We collected two types of outcomes: clinical and cost-related.
We wanted to analyse the effectiveness of ReHand not only from a clinical perspective, but also from the perspective of shortening patient recovery and its impact on the healthcare system. Some outcomes were, for example, return-to-work days or self-reported functional ability.
Did the tablet-based approach hasten return to work?
Yes, patients treated with ReHand returned to work earlier, specifically an average of 18 days (95% CI –33 to –3) earlier than patients treated with conventional exercise programs.
What about healthcare usage?
Healthcare usage (ie, sessions and consultations) was also reduced in the ReHand treatment group, which makes sense since patients were recovering earlier.
However, I would like to emphasise the impact of ‘hastening return to work’ on healthcare usage.
Off-work days are a cost for public systems, and also for companies.
For example, in previous research about tendon transfers in the German healthcare system, the cost per off-work day was US$50.
Thus, just by hastening the patient recovery in one day, a saving of US$50 per patient would be generated.
Were the clinical outcomes the same in the two groups?
No, clinical outcomes such as self- reported functional ability at Week 2 and pinch strength at Week 2 favoured the experimental groups.
Although the rest of the clinical outcomes had mean estimates that favoured the experimental intervention at Week 2 and 4, confidence intervals were too imprecise to clearly indicate whether the true effect was beneficial.
Do you think the benefits of the tablet-based system outweigh its extra cost and organisation?
This is a question that should be answered by health professionals and health systems themselves.
On the one hand, we health professionals must ask ourselves if it is worth investing time and money in the implementation of health technology for our patients in our clinic.
To do this, we must assess what each technological solution brings in terms of improving care procedures, optimising the logistics of clinical practice, enhancing patient outcomes, and generating competitive differentiation from other clinics and professionals.
Moreover, the COVID period is teaching us that new strategies that empower patients and make him/her participate in their recovery process are needed. Some technological solutions enable this, while allowing for work both in the clinic and at home.
On the other hand, health systems need health innovations that enable them to optimise healthcare and patient monitoring.
In certain cases, this also translates into faster recovery and savings, which improves the sustainability of the health system.
Your research group achieved similarly beneficial effects from the ReHand system in people after carpal tunnel surgery. Are you looking at other clinical groups?
Yes, we are expecting to publish new clinical results focused on specific pathologies such as distal radius fracture or soft tissue injuries.
Furthermore, in the medium term we would like to publish sensitivity and specificity studies about ReHand’s predictive system, a set of algorithms that predicts the clinical evolution of patients based on all the data collected by ReHand from each patient.
María-Dolores Cortés-Vega, PhD, is a professor in the physiotherapy department at the Faculty of Nursing, Physiotherapy and Podiatry, University of Seville, Spain. Her research focuses on exercise therapy, virtual reality and inclusive education in higher education.
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.





