
Exploring sustainable advanced practice physio across international boundaries

As part of her Winston Churchill Memorial Trust Fellowship, UK-based physiotherapist Hannah Morley visited advanced practice services in Australia and New Zealand in early 2020, enabling her to make an international comparison of the development and implementation of advanced practice.
Advanced practice physiotherapy (APP) is underpinned by the four pillars of advanced practice: clinical practice, leadership, research and educational (Chartered Society of Physiotherapy 2020).
Advanced physiotherapy practitioners (APPs) are involved in high-level, complex decision-making to inform diagnosis, investigation, management and onward referral for patients. APPs enable, facilitate, and support change across care pathways and across traditional professional and organisational boundaries.
Internationally, APP is accessed in different ways depending on the structure of the health service and in which context APPs can be found. APP roles are commonly found in primary care, emergency departments and orthopaedic clinics (Williams et al 2019).
The differences and similarities in APP services and roles across the UK, Australia and New Zealand were explored in this Winston Churchill Memorial Trust (WCMT) Fellowship.
The WCMT project explored how APP has been implemented and the challenges, successes and shared learning discovered across different countries, regions and services.
This article is a summary of that project and will focus on the small changes individual clinicians can make in their own practice or service.
The full WCMT report, ‘Exploring the efficacy of Advanced Practice in physiotherapy: an international comparison’, makes several recommendations that individuals, services, regions or nations can take to improve the sustainability and efficiency of APP services and roles.
This report can be accessed on the WCMT website here.
Methodology
A Churchill Fellowship is a unique research grant that supports citizens to investigate innovative solutions for today’s most pressing problems through practical inquiries into real-world issues.
The focus of a Churchill Fellowship is to travel to areas with different approaches in order to learn from one another.
This WCMT Fellowship carried two objectives:
- to investigate the challenges, successes and shared learning around the implementation of APP in New Zealand and Australia
- to make recommendations for practice for APPs and APP services.
An initial scoping exercise was conducted, performing a literature search and engaging in discussions with experts in the field within the UK.
This scoping identified a number of key sites and services of interest.
Themes emerging from this scoping included clinical governance and regulation, education and training, and clinical innovation, and these were used to inform the template for semi-structured interviews, which were recorded using dictation software.
Sites were chosen due to practical considerations such as contact, willingness and availability of site staff, funding limitations and time available.
Clinicians and system leaders from these sites were interviewed about their contributions to and experiences of APP.
These visits often involved meeting with teams from these services, observing clinical interactions and training events, touring facilities and sharing useful resources such as research papers and local policies.
After data collection, transcription and thematic analysis was conducted. Initial findings emerged from this analysis and were shared with contributors to ensure accuracy.
Findings
The overarching themes that emerged from the data collection and analysis included clinical governance, regulation, education, digital and technology, leadership, research, culture, integrated care and roles.
Table 1 details the findings within five of these overarching themes. Full findings are available in the full report mentioned above.

Table 1.
Discussion
Sustainability of APP roles and services was an area that contributors were very keen to discuss, particularly how the need for sustainability had influenced their service developments and innovations.
Contributors outlined how clear principles, vision and values made decisions and choices for innovation and improvement easier.
Having a strong understanding of the mission behind their services such as citizen engagement, cultural competence and shared decision-making was important for system leaders and clinicians.
These principles, visions and values were thought to be important factors that helped form the strategic direction of APP services and roles.
The process and system of an APP service was also important in its sustainability.
The perception that peers, colleagues and patients had about APP was key to overcoming barriers and communicating the principles, values and vision was crucial to this.
Education was felt to be an important factor in the sustainability of APP.
Contributors detailed the innovative educational solutions they had implemented in order to develop the future workforce.
It was felt that clear career pathways with robust educational programs would benefit the workforce long term and support retention and recruitment in the short term.
Educational programs which were portable across organisations and regions were also an important factor for clinicians.
Increased access to APP services through use of telehealth and proliferation APP services helped to support a more positive perception.
Mentorship, supervision and peer networks also contributed to the clinicians’ sustainable tenure.
Based on the findings above, Table 2 gives recommendations for promoting and maintaining sustainable APP roles and services.
These recommendations are intended for the reader to use as a springboard for initiating conversations about change in their own workplace and within their sphere of influence.
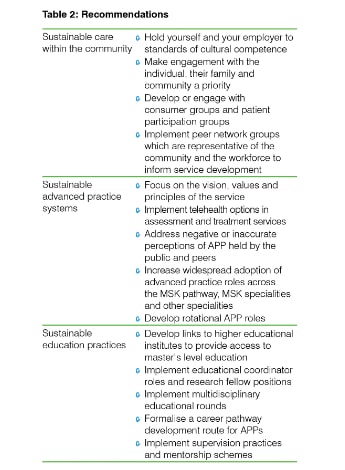
Table 2.
Conclusion
This project has demonstrated the similarities and differences in the challenges, successes and lessons of implementing, maintaining and developing sustainable APP roles and services across international boundaries.
This project was a small scale exploratory piece of work which highlights the need for further research to understand the barriers, challenges and possible solutions for sustainable APP within the wider healthcare systems.
This project also highlighted the value of APP to patients, staff, services and organisations, and more research in this area may provide further advancement for the physiotherapy profession internationally.
Hannah Morley is an advanced practice physiotherapist and first contact practitioner from Gloucestershire and Bristol in the UK. Hannah travelled to Australia and New Zealand to research the implementation and development of advanced practice within physiotherapy. Her findings have been used to inform workforce planning, educational strategies and governance development for physiotherapists in the UK.
- References
Chartered Society of Physiotherapy. 2020. Advanced Practice Physiotherapy. [online] Available at: https://www.csp.org.uk/system/files/csp_advanced_practice_physiotherapy_... [Accessed 12 April 2020].
Williams, A. Stotter, G. Hefford, C. Waaren, J. Darlow, B. 2019. Impacts of advanced physiotherapy: A narrative literature review. New Zealand journal of physiotherapy. 3, pp. 150 [Accessed 10 Jan 2019]
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.





