
Mixed headache presentation with neck pain

Harry Truong presents a case study of a 42-year-old patient with a mixed headache presentation and neck pain and details the biopsychosocial approach to treatment.
Headaches are a common condition, affecting 47 per cent of the global population with a lifetime prevalence estimated to be more than 90 per cent (Stovner et al 2007).
Headaches can negatively affect a person’s quality of life and functional capacity.
There are many forms of headache, which are broadly classified into three types: primary headaches, secondary headaches and cranial neuralgias according to the International Headache Society (International Headache Society 2018).
Primary headaches are the most common and are often defined as idiopathic—without a known identifiable cause or disease process.
Secondary headaches are associated with a disorder or pathology that can be identified. These include cervicogenic headache (CGH), temporomandibular-related headache and those associated with more serious pathology such as tumour and stroke.
The most common primary headache types are tension-type headache (TTH) (42 per cent) and migraine (11 per cent; Stovner et al 2007, Steiner et al 2003).
Given each headache form has a different pathogenesis, incorrect differential diagnosis will often lead to ineffective management.
It is well known, however, that diagnostically, there is symptomatic overlap between different headache types, particularly migraine, TTH and CGH (Turkdogan et al 2006, Liang et al 2019, Luedtke et al 2018, Watson & Drummond 2012).
Neck pain is commonly associated with headache, with as many as 60 to 80 per cent of those experiencing migraine and TTH also reporting neck pain (Liang et al 2019, Luedtke et al 2018, Watson & Drummond 2012, Jull et al 2019).
The purpose of this case study is to explore the assessment and management of a patient who presented with longstanding headache and neck symptoms with overlap between different headache forms. Informed consent was gained prior to the writing of this case study.
Presentation
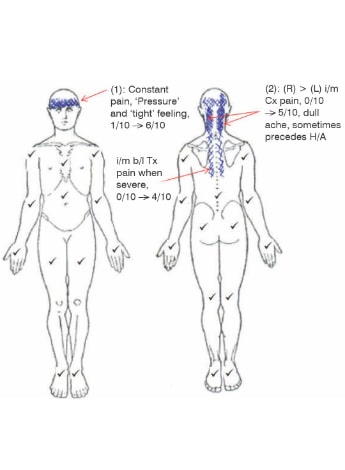
A 42-year-old male presented with an 18-month history of persistent bilateral frontal headache with bilateral neck pain, which would intermittently radiate along his thoracic spine when his pain was severe (Figure 1 below).
On presenting history, he reported an initial gradual worsening of headache and neck pain while at work as a bus driver, towards the end of a particularly long and stressful shift, about 18 months ago.
Since then, he reported experiencing almost-daily headaches and intermittent neck pain which has worsened with frequency and duration, but not intensity.
Furthermore, he reported a longstanding 20-year history of the same intermittent headache and neck pain of no specific onset before immigrating to Australia from Afghanistan four years ago.
His main headache symptoms were described as a ‘pressure’ feeling around his head that would last for one to two hours and were generally constant with periodic exacerbations.
He would experience these five to seven days per week, particularly during workdays, and would get accompanying bilateral neck pain.
These symptoms were aggravated with sustained postures such as sitting and driving more than 20 minutes and carrying more than 20kgs.
He reported that increased stress would trigger these headache and neck symptoms and would particularly notice symptoms at the end of a work shift.
Intermittently throughout the week, he would experience right neck pain which would precede right-side dominant headache.
This would be aggravated with prolonged or repeated cervical right rotation when driving. Symptoms were never isolated and were variable in duration, ranging from minutes to a few hours.
The patient reported no symptoms suggestive of any sinister pathology or any other possible associated symptoms such as dizziness, jaw pain, nausea, vomiting, and photo or phonophobia.
He described an intermittent feeling of fatigue in his shoulders during driving when his headache symptoms were severe.
Easing factors included heat and massage and going for a walk provided temporary relief. He reported pain-relief medications were no longer of benefit.
The patient reported feeling well in the mornings but would usually have a headache by the end of day. He reported he generally did not sleep well, averaging about five hours of broken sleep due to stress and that his mind was ‘always thinking and worrying’.
The patient was slightly overweight with a history of high cholesterol, blood pressure and Type 2 diabetes, which were controlled with medication.
He reported a history of depression which was controlled by medication (Zoloft 100mg a day). The patient reported no other significant health concerns.
Management by his treating GP included X-ray and CT scans of his cervical spine, which were unremarkable. He had seen multiple health professionals, including physiotherapists, and management was predominantly passive therapies without any long-term benefit.
The patient’s priorities were pain relief and to reduce headache symptoms and frequency, as they were affecting his work and family life.
He reported he was becoming easily agitated when he had a headache and was reducing social participation.
In addition, there were ongoing stressors concerning safety of his extended family back home. He is married with a supportive wife and five teenage children, and as the sole income provider, has continued to work full-time. He was not participating in a regular exercise program.
Self-reported outcome measures were administered on initial visit and showed high disability on the Headache Impact Test-6 (HIT-6; Houts et al 2019), Patient-Specific Functional Scale (Hefford et al 2012), DASS-21 (Henry & Crawford 2005) and short form Orebro (Hockings et al 2008; Table 1 here).
Objective examination
- Main physical assessments findings were:
- bilateral neck pain and headache 4/10 at rest on Numerical Rating Scale (NRS)
- resting standing posture showed increased thoracic kyphosis, forward head posture (FHP) with downward rotation of bilateral scapulae. Resting sitting posture exaggerated these findings
- full active shoulder flexion and abduction bilaterally with observed poor eccentric control of bilateral scapulae on return functional assessment of replicating his seated driving position holding two 2kg dumbbells in each hand further accentuated his FHP and thoracic kyphosis, with increased bilateral scapulae winging and produced ‘tension’ in his neck and increased his headache:
- active correction of cervico-thoracic and scapulae position to neutral improved his symptoms but he had difficulty maintaining the position due to reported fatigue
- ° passive correction of scapula-thoracic position also improved his symptoms
Main range of motion (ROM) findings were:
- upper cervical flexion pain-free but extension increased right sided neck symptoms
- right cervical rotation 40 degrees, with increased right cervical pain and right-sided headache
- ° improved to 60 degrees and decreased symptoms with active scapula-thoracic correction to neutral
- left rotation 70 degrees with no pain, but improved to 85 degrees with correction as above
- extension 20 degrees with observed poor movement pattern on return (no cranio-cervical flexion)
- thoracic extension was limited on active and passive assessment
- Flexion-Rotation Test (FRT; Hall et al 2010) to right was 20 degrees and left 45 degrees
- passive physiological assessment of the cervical segments showed restriction in movement of the upper cervical segments on the right C1/2 to C3/4.
- passive accessory intervertebral movement assessment reproduced headache over the right C1/2 and was tender over the C2/3 and C3/4 levels and was generally hypomobile through his thoracic spine:
- symptoms were reduced following activation of scapula muscles
- palpation: generalised pericranial tenderness over upper cervical extensors, temporalis, scapular elevators as well as anteriorly over scalenes and sternocleidomastoid
- neurodynamic testing of slump and upper cervical flexion with straight leg raise and upper limb tension testing was negative
- axioscapular muscle assessment showed impaired endurance bilaterally on prone scapular holding testing and wall push up testing (Jull et al 2019), with reported increased effort and inability to maintain scapula control during testing
- cranio-cervical flexor endurance assessment by head lift was four seconds before fatigue with observed excessive superficial muscle activation. Normative data for males being 39 seconds test (Domenech et al 2011)
- cervical extensor endurance testing in quadruped position (Jull et al 2019): five repetitions before losing cranio-cervical and neutral scapula position (Table 2 here).
Management
Initial management focused on education regarding his diagnosis, treatment planning and discussion of prognosis considering the long-standing nature of his symptoms and influence of psychosocial factors such as stress.
Following discussion with the patient, he was recommended to see a psychologist to provide cognitive interventions and assist with relaxation and stress management.
Physiotherapy management was targeted towards addressing the articular and muscular impairments found in the physical assessment.
Targeted manual therapy was used to provide initial pain relief as an adjunct to a graduated motor control and strengthening program (Table 3 here) in management.
Studies have shown that a combination of manual therapy and motor control exercises is more effective than GP care for chronic TTH (Castien et al 2010, Mesa-Jiménez et al 2015) and is effective in reducing frequency and intensity of CGH (Jull et al 2002).
Passive mobilisations (posterior-anterior Maitland mobilisations) were applied to the pain-sensitive cervical segments (C1/2 to C3/4) with good effect, reducing headache intensity and neck symptoms.
Soft tissue massage was used to help reduce muscular tension and facilitate relaxation. The aims of the graduated exercise program were to:
- develop cranio-cervical and cervical extension control
- improve strength and endurance of both cervical and scapulo- thoracic regions
- encourage a regular routine of cardiovascular exercise to facilitate stress management and promote general wellbeing.
In adopting a biopsychosocial approach to management, ongoing discussion and recommendations were provided about sleep hygiene, encouragement to return to regular social and family outings and adopting a more balanced lifestyle incorporating regular exercise.
Initially, a low-load program was prescribed—motor control exercises targeting the deep cervical flexors and postural cues to improve scapulo-thoracic position as home exercises.
These were prescribed as they improved symptoms and range during assessment. A daily graded walking program was prescribed to encourage regular exercise, as the patient reported walking improved his symptoms.
The home exercise program was gradually progressed to a higher load program aimed at targeting scapulo-thoracic strength and cervical flexor and extensor endurance. Exercises were progressed through load and complexity.
Parameters were prescribed at the repetition level where the patient could no longer maintain appropriate control or range during assessment. Pain levels post-exercises were also monitored.
Exercises were performed during consultation to ensure correct technique and to monitor symptom response.
The home exercises were initially completed daily, but was progressed to two to three times per week for the strength and endurance program.
He reported he did not have time to attend a local gym, but opted to self-manage through a combination of home exercises, walking and utilising outdoor equipment at a local park.
Outcomes
The patient was seen 14 times over a four-month period. He reported a significant improvement in neck pain, and no longer reported any thoracic symptoms.
The patient still reported experiencing ongoing headaches—but intensity and frequency were improved and he was happy to self-manage. There were improvements across all clinical assessment and self-reported outcome measures (Tables 1 here and 2 here).
He continued to work full-time throughout his rehabilitation but was now also successfully maintaining a regular exercise routine—a combination of walking and home exercises or intermittent use of a local park with outdoor fitness equipment.
He was also regularly seeing his psychologist for follow-up.
Discussion
Diagnosis—the patient’s diagnosis was a mixed headache presentation.
According to the International Classification of Headache Disorders (ICHD-3), the patient’s symptoms fulfilled criteria suggestive of a frequent episodic TTH—his symptoms were bilateral, non-pulsating quality of mild-moderate intensity with no associated symptoms of nausea and photo or phonophobia and were not aggravated by physical activity, with at least 10 episodes per month for longer than three months.
He also presented with pericranial tenderness on palpation which can often be present in TTH (Fernández-de-las-Peñas et al 2007).
A recent systematic review reported that TTH presented with more cervical impairments than in migraine (Liang et al 2019).
The patient’s cervical impairments, however, were also suggestive of CGH. He had reduced cervical rotation range and limited right FRT (Hall et al 2010), along with palpatory findings which reproduced his headache, and impairment in his cranio-cervical muscles on head lift test (Domenech et al 2011).
A cluster of these three physical findings (reduced ROM, painful upper cervical joint dysfunction on manual examination and impairment in cranio- cervical muscle function) has been shown with 100 per cent sensitivity and 94 per cent specificity to identify neck dysfunction associated with CGH (Jull et al 2007), which was also validated in a recent study (Getsoian et at 2020).
Amiri et al (2007) found that patients with a mixture of migraine and TTH did not demonstrate the presence of this cluster described above (Amiri et al 2007); however, as there is often symptomatic overlap between different headache forms (Jull et al 2019, Bogduk & Govind 2009) his headache symptoms were suggestive of both TTH and CGH.
Management—contributing factors to his presentation included poor endurance of his axioscapular muscles and cranio-cervical flexors and extensor muscles, on the background of psychosocial factors (ongoing stress, depression and poor sleep).
Given the patient’s poor long-term response to passive therapies, the main aims of management were to promote self-management and adopt an active approach.
Despite mixed evidence for the effectiveness on certain headache types, physiotherapy management has been shown to be effective in reducing intensity of TTH and both intensity and frequency of CGH (Luedtke et al 2015).
Manual therapy in this case was applied for initial pain relief as it provided the patient with a positive response in symptoms and has been shown to reduce trigemino-cervical nucleus (TCN) sensitivity (Watson & Drummond 2014).
The patient’s neck pain appeared to be both an associated symptom of his headache but also potentially a contributing source of CGH, given the cervical muscles and their attachment to the upper cervical vertebrae and the assessment findings of articular impairment of the upper cervical segments.
In this case, the relief provided from manual therapy and exercising of the cranio-cervical and axioscapular muscles warranted targeted treatment of this area.
Exercises targeting postural correction and endurance-based cranio-cervical and axioscapular exercises were prescribed based on the impairments found on assessment, being either below normative values (Domenech et al 2011), and with increased effort and/or poor control.
Jull et al (2002) found that exercises targeting both deep neck flexor and axioscapular muscles improved CGH symptoms.
The pathophysiology of TTH remains unclear, though studies have reported both peripheral mechanism and central mechanisms may explain some of the symptoms (Bendtsen 2000).
As sensitisation of the TCN is an important factor in headache generation (Bogduk & Govind 2009, Bogduk 2004, Castien & De Hertogh 2019, Chua et al 2011), a person’s biological, psychological, social and contextual factors attached to their headache and pain experience all contribute to how much the central nervous system becomes sensitised (Jull et al 2019).
Poor sleep, lack of exercise and stress can contribute to ongoing symptom amplification (Nijs et al 2017).
Given the patient scored high on the DASS-21, had a longstanding history of depression, reported a correlation between stress and his symptoms, along with a lack of exercise and an increased impact on his social participation—the presence of these psychosocial elements needed to be addressed in his management.
A recent systematic review supported psychological treatment for primary headache disorders (Lee et al 2019) and showed effectiveness in managing concomitant psychological distresses.
In this case, a whole-person approach along with psychological management helped in improving the patient’s overall outcome.
Despite improvement in clinical assessments, outcome measures and willingness for the patient to self-manage, a follow-up review would have been ideal to monitor long-term progress but due to the current environment (COVID-19 pandemic), the patient declined and was happy to self-manage.
Limitations to this study included lack of availability of a pressure biofeedback unit to provide quantitative measures of the deep neck flexors on assessment through the cranio-cervical flexion test.
This would have assisted with making reassessment measurements more sensitive to change.
Conclusion
This case illustrates the importance of adopting a biopsychosocial framework in assessing and managing patients presenting with headache.
A collaborative and patient-centred approach, matching physiotherapy goals with individual patient goals, ensures effective holistic patient management.
>> Harry Truong is an APA Musculoskeletal Physiotherapist and an APA Sports and Exercise Physiotherapist currently undertaking Fellowship of the Australian College of Physiotherapists by Clinical Specialisation in musculoskeletal physiotherapy. Harry works clinically at ProHealthCare and is an educator in the physiotherapy program at the University of South Australia.
- References
References
1 Stovner LJ, Hagen K, Jensen, R, Katsarava, Z, Lipton, RB, Scher, AI, Steiner, TJ & Zwart, JA 2007 ‘The global prevalence and disability worldwide, Cephalalgia, vol. 27, pp. 193-210.
2 International Headache Society 2018, International Classification of Headache Disorders (ICHD) 3rd edition, viewed 15 June 2020, https://ihs-headache.org/wp-content/uploads/2020/05/ICHD-3-Pocket-versio....
3 Turkdogan, D, Cagirici, S, Soylemez, D, Sur, H, Bilge, C & Turk, U 2006 ‘Characteristic and overlapping features of migraine and tension-type headache’, Headache, vol. 46, pp. 461-468.
4 Liang, Z, Galea, O, Thomas, L, Jull, G & Treleaven, J 2019 ‘Cervical musculoskeletal impairments in migraine and tension type headache: a systematic review and meta-analysis’, Musculoskeletal Science and Practice, vol. 42, pp. 67-83.
5 Luedtke, K, Stark, W & May, A 2018 'Musculoskeletal dysfunction in migraine patients', Cephalalgia, vol.38, pp.865–875.
6 Watson, D & Drummond, P 2012'Head pain referral during examination of the neck in migraine and tension-type headache', Headache, vol. 52, pp.1226–1235.
7 Steiner, TJ, Scher, AI, Stewart, WF, Kolodner, K, Liberman, J & Lipton RB 2003 'The prevalence and disability burden of adult migraine in England and their relationships to age, gender and ethnicity' Cephalalgia, vol. 23, no. 7, pp 519-527.
8Houts, CR, Wirth RJ, McGinley, JS, Gwaltney, C, Kassel, E, Snapinn, S & Cady, R 2019 ‘Content validity of HIT-6 as a measure of headache impact in people with migraine: a narrative review’, Headache: The Journal of Head and Face Pain, vol. 60, no. 1, pp. 28-39.
9 Hefford, C, Abbott, JH, Arnold, R & Baxter, GD 2012,'The patient-specific functional scale: validity, reliability, and responsiveness in patients with upper extremity musculoskeletal problems', Journal of Orthopaedic & Sports Physical Therapy, vol. 42, no. 2, pp. 56-65.
10 Henry, JD & Crawford, JR 2005 'The short-form version of the Depression Anxiety Stress Scales (DASS-21): construct validity and normative data in a large non-clinical sample', British Journal of Clinical Psychology, vol. 44, pp. 227-239.
11 Hockings, RL, McAuley, JH & Maher, C 2008 ‘A systematic review of the predictive ability of the Orebro Musculoskeletal Pain Questionnaire’, Spine, vol. 33, no. 15, pp. e494- e500.
12 Hall, T, Briffa, K, Hopper, D, & Robinson, K 2010 ‘Long-Term Stability and Minimal Detectable Change of the Cervical Flexion-Rotation Test. Journal of Orthopaedic & Sports Physical Therapy, vol. 40,no. 4, pp. 225–229.
13 Jull, G, Falla, D, Treleaven, J & O’Leary, S 2019, Management of neck pain disorders: a research informed approach, Elsevier, Edinburgh.
14 Domenech, MA, Sizer, PS, Dedrick, GS, McGaillard, MK & Brismee JM 2011, 'The deep neck flexor endurance test: normative data scores in healthy adults', Physical Medicine and Rehabilitation, vol. 3, pp. 105-110.
15 Bendtsen, L 2000 'Central sensitization in tension-type headache: possible pathophysiological mechanisms', Cephalalgia, vol. 20, pp. 486-508.
16 Bogduk, N & Govind, J 2009, ‘Cervicogenic headache: an assessment of the evidence on clinical diagnosis, invasive tests, and treatment’, Lancet Neurology, vol. 8, pp. 959-968.
17 Bogduk, N 2004 ‘The neck and headaches’, Neurosurgery Clinics of North America, vol. 22, pp. 151-171.
18 Castien, R & De Hertogh, W 2019 ‘A neuroscience perspective of physical treatment of headache and neck pain’, Frontiers in Neurology, vol. 10, no. 276, pp. 1-7.
19 Jull, G, Amiri, M, Bullock-Saxton, J, Darnell, R & Lander, C 2007 'Cervical musculoskeletal impairment in frequent intermittent headache: part 1: subjects with single headaches', Cephalalgia, vol. 27, pp. 793-802.
20 Getsoian, SL, Gulati, S, Okpareke, I, Nee, RJ & Jull, G 2020 'Validation of a clinical examination to differentiate a cervicogenic source of headache: a diagnostic prediction model using controlled diagnostic blocks', British Journal of Medicine Open, vol. 10, pp. 1-9.
21 Amiri, M, Jull, G, Bullock-Saxton, J, Darnell, R & Lander, R 2007 ‘Cervical musculoskeletal impairment in frequent intermittent headache: part 2: subjects with concurrent headache types’, Cephalalgia, vol. 27, pp. 891-898.
22 Fernández-de-las-Peñas, C, Cuadrado, M, Arendt-Nielsen, L, Simons, D & Pareja, J 2007 'Myofascial trigger points and sensitization: an updated pain model for tension-type headache, Cephalalgia, vol. 27,no. 5, pp. 383–393.
23 Luedtke, K, Allers, A, Schulte, LH & May, 2015 ‘Efficacy of interventions used by physiotherapists for patients with headache and migraine – systematic review and meta-analysis’, Cephalalgia, vol. 36, no. 5, pp. 474-492.
24 Castien, RF, van der Windt, DA, Grooten, A & Dekker, J 2010 ‘Effectiveness of manual therapy for chronic tension-type headache: a pragmatic, randomised, clinical trial’, Cephalalgia, vol. 31, no. 2, pp. 133–143.
25 Mesa-Jiménez, JA, Lozano-López, C, Angulo-Díaz-Parreño, S, Rodríguez-Fernández, ÁL, De-la-Hoz-Aizpurua, JL, & Fernández-de-las-Peñas, C 2015 ‘Multimodal manual therapy vs. pharmacological care for management of tension type headache: a meta-analysis of randomized trials’, Cephalalgia, vol. 35, no. 14, pp. 1323–1332.
26 Jull, G, Trott, P, Potter, H, Zito, G, Niere, K, Shirley, D, Emberson, J, Marschner, I & Richardson, C 2002 ‘A randomized controlled trial of exercise and manipulative therapy for cervicogenic headache’, Spine, vol. 27, no. 17, pp. 1835-1843.
27 Watson, D & Drummond, PD 2014 ‘Cervical referral of head pain in migraineurs: effects on nociceptive blink reflex’, Headache, vol. 54, pp. 1035-1045.
28 Nijs, J, Loggia, ML, Polli, A, Moens, M, Huysmans, E, Goudman, L, & Clauw, D 2017 ‘Sleep disturbances and severe stress as glial activators: key targets for treating central sensitization in chronic pain patients?’, Expert Opinion on Therapeutic Targets, vol. 21, no.8, pp. 817–826.
29 Chua, NH, van Suijlekom, HA, Vissers, KC, Arendt-Nielsen, L & Wilder-Smith, OH 2011 ‘Differences in sensory processing between chronic cervical zygapophysial joint pain patients with and without cervicogenic headache’, Cephalalgia, vol. 31, no. 8, pp. 953-963.
30 Lee, HJ, Lee, JH, Cho, EY, Kim, SM & Yoon, S 2019 ‘Efficacy of psychological treatment for headache disorder: a systematic review and meta-analysis’, The Journal of Headache and Pain, vol. 20, no. 17.
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





