5 Facts about physiotherapy and sports-related concussion
Dr David Munro of the APA Sports and Exercise national group presents five discussion points about the aetiology, prevention and management of sports-related concussion.
1. The definition of concussion has evolved over time

A concussion occurs through a collision with another person or object where biomechanical forces to the head, or anywhere on the body, transmit an impulsive force to the brain, resulting in transient neurological impairment.
It is worth noting that concussion can occur with relatively minor physical interactions (Patricios et al 2023).
Concussion is an evolving condition and symptoms can change over the hours or days following an injury (McCrory et al 2016, Bretzin et al 2018).
There are often adverse effects on balance and cognitive function (McCrory et al 2016).
Pathophysiological recovery may take longer than measures of clinical recovery (Kamins et al 2017) and the average time taken to resolve clinical symptoms may vary according to sex, age, the presence of pre-injury medical conditions and para-athlete status (Bretzin et al 2018, Weiler et al 2018, Chandran et al 2020, Black et al 2017).
The current clinical definition of concussion does not distinguish persistent symptoms, the underlying processes that impair brain function or any potential brain abnormalities.
To overcome this limitation, the Concussion in Sport Group’s sixth consensus statement noted that ‘symptoms and signs may present immediately, or evolve over minutes or hours, and commonly resolve within days, but may be prolonged’ (Patricios et al 2023).
2. Women are at higher risk of concussion

The risk of concussion is higher in female athletes than in male athletes (Abrahams et al 2014, McGroarty et al 2020) and women experience worse outcomes from prolonged symptoms (Black et al 2017, Abrahams et al 2014, McGroarty et al 2020).
While the evidence is currently limited, many hypotheses exist as to why concussion is more common in women.
One hypothesis is a lower biomechanical threshold tolerance for head impacts in women, resulting in more severe symptomatology (McGroarty et al 2020).
Factors such as lower neck strength may also predispose women to greater head/neck acceleration during impact, increasing the risk of concussion (McGroarty et al 2020).
A link is emerging between progesterone levels and the risk and outcomes of concussion (Di Battista et al 2019, La Fountaine et al 2019, Wunderle et al 2014).
For instance, the risk of concussion is higher during the late luteal phase of the menstrual cycle (high progesterone concentration) and during the first two days of menstruation (La Fountaine et al 2019).
Those who sustained a concussion during the luteal phase of their menstrual cycle also report higher incidences of negative quality-of-life outcomes and neurological symptoms after one month (Wunderle et al 2014).
3. Concussion pathophysiology is not fully understood
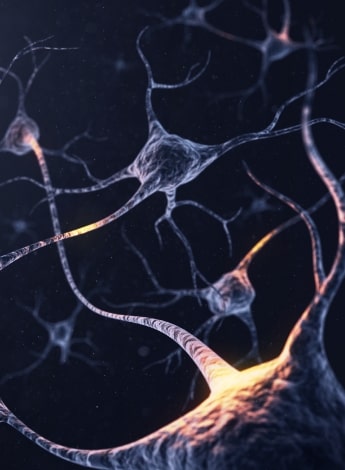
The pathophysiology of concussion is complex and multifactorial.
Despite a large global increase in research in this area over the past 20 years, the underlying process is not yet completely understood.
Current thinking is that the initial biomechanical impact can initiate a cascade of events that results in abnormal function at the cellular level.
There is evidence that shearing experienced by the brain can alter blood flow to brain tissue, affecting metabolism and membrane permeability, releasing excessive neurotransmitters and causing neuroinflammation (Steenerson & Starling 2017).
It is thought that biomechanical forces cause neuronal cell membrane disruption and axonal stretching.
During a head impact, gelatinous grey matter undergoes significant shear forces from sudden acceleration and deceleration and pulling or pushing of brain tissue can cause structural damage.
The ion channels on the cell membranes become dysregulated and allow an indiscriminate flux of ions.
Potassium efflux and calcium influx cause depolarisation, leading to the release of glutamate, an excitatory neurotransmitter.
Attempting to restore the resting membrane potential, ATP-dependent membrane ion pumps then become overactive.
This increases glucose demand, resulting in a temporary depletion of intracellular energy reserves.
There may also be a reduction in cerebral blood flow during this time, further affecting the energy shortage (Giza & Hovda 2014).
4. Clinical features of concussion can vary widely

Concussed athletes may exhibit a wide range of signs and symptoms.
There is no ‘typical concussion’ and accurate and timely diagnosis can be challenging due to a lack of definitive diagnostic markers or investigations and the overlap of symptoms with other neurological, musculoskeletal and psychological diagnoses.
Concussion is therefore a clinical diagnosis based on the individual’s history, symptoms and signs on physical examination (McCrory et al 2016).
A key concept in on-field assessment is rapid screening for a suspected concussion rather than focusing on the definitive diagnosis of head trauma.
A concussion evaluation is triggered in contact and collision sports when an athlete experiences a direct or indirect impact to their head and/or trunk associated with visible signs of a concussion and/or the athlete reports symptoms and/ or there is clinical suspicion by medical staff and/or a possible concussion event is reported by match officials.
The Sport Concussion Assessment Tool-6 and Sport Concussion Office Assessment Tool-6 are the current recommended tools for concussion assessment (Patricios et al 2023).
Clinicians should also consider baseline testing for athletes and teams with higher risks of concussion.
As well as being useful in the clinical diagnosis of concussion, baseline testing may help guide appropriate rehabilitation and return-to-sport decision-making.
5. Physiotherapy plays an important role in prevention and management

There is increasing evidence to support the involvement of physiotherapists in the assessment and management of concussion (Brown & Camarinos 2019).
In addition to delivering concussion education and prevention sessions to athletic groups, it is often a physiotherapist who will recognise a suspected concussion and be responsible for removing an athlete from the field of play.
Most concussion cases are uncomplicated and 70–80 per cent of people recover within expected time frames, requiring minimal clinical input (Makdissi et al 2013, Collins et al 2014, Lyons et al 2022, Davis et al 2022, Quatman-Yates et al 2020).
However, up to 30 per cent of concussion cases are more complex, with prolonged symptoms and recovery (Makdissi et al 2013, Lyons et al 2022, Davis et al 2022).
Physiotherapists play a crucial role in complex case management, including further clinical review of patients who do not progress as expected through the graded return to sport or are identified as having vestibular and/or oculomotor dysfunction.
Several studies demonstrate that appropriate rehabilitation delivers faster symptom resolution, faster return to function and a more complete recovery, highlighting the significant contribution that physiotherapists can make to concussion management (Brown & Camarinos 2019, Broglio et al 2015, Kontos et al 2017, Lumba-Brown et al 2020).
Quick links:
- References
- Infographic poster of this article.
COURSE OF INTEREST: Sports-related concussion: the role of physiotherapy in acute care, rehabilitation and safe return to play here.
>> Dr David Munro APAM is the head physiotherapist at the National Institute of Circus Arts and a member of the APA Sports and Exercise national group. David was part of an APA working group contributing to the Australian Institute of Sport’s Concussion and Brain Health Position Statement 2023.
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.