Research examines painful truth about knee OA
In this second instalment of a two-part series on knee osteoarthritis and conservative management in the public setting in Canberra, Professor Jennie Scarvell discusses a research project that is helping to reshape the care pathway.
Around the time that a pioneering program to filter public patients through a conservative management program for knee osteoarthritis (OA) in Canberra was finding its feet, a research project at the University of Canberra (UC) was also getting underway.
Each project had a similar goal—to avoid costly knee replacement surgery when it was unnecessary and to reduce the waiting time for those who did need surgery.
The Good Life with osteoArthritis Denmark (GLA:D) program, introduced through Canberra Health Services in 2021, was already making significant inroads when the UC research program ‘Best practice knee osteoarthritis embedding advanced physiotherapy in orthopaedic screening’, overseen by chief investigator and physiotherapist Jennie Scarvell APAM, was rolled out to ensure that patients with hip and knee OA have access to the non- surgical interventions they need.
The two-year, private health insurer HCF-funded translation project boasts a team of 12 investigators and is run in collaboration with Canberra Health Services, community and acute care physiotherapists and the orthopaedic surgery team at Canberra Hospital.
The success of the GLA:D program and the funding of the research project created an opportunity for all interested parties to come together to see if improvements could be made to the clinical care pathway for people with OA.
Jennie, deputy dean at the Faculty of Health and leader of the Clinical Research Rehabilitation and Translation group at UC, is the lead on the research project.
She says the project came about in part because public patients with knee OA in Canberra had been missing out on conservative management.
In many instances, GPs were steering patients onto the surgical pathway before those patients had considered or participated in any conservative management.
‘On the surgical pathway, the GPs refer to the orthopaedic surgery team; the patient sees a surgeon; they get a knee replacement,’ Jennie says.
‘So Canberra Health Services has put advanced physiotherapy practitioners into triage and screening. We started off with the physios doing triage.
'If the referrals were incomplete, the physios could send the referrals back to the GP and get more information.
‘The next stage was for the advanced practice physios to undertake screening and they were screening patients that they thought, based on their GP referrals, were likely to be unsuitable for surgery because they hadn’t yet exhausted non-surgical interventions.
'There was a high risk of those patients being rejected by the surgeons, who were discharging 27 per cent of the patients they saw at that stage.
'The advanced practice physios then screened all the patients with knee pain and the discharge of surgery rate is now down to 10 per cent.
'The surgeons are getting more appropriate patients coming through to them and a lot more patients are now going on to have non-surgical management.’
The research team undertook a series of 27 interviews with health services personnel, GPs, surgeons and patients to garner their level of understanding of the GLA:D program.
Jennie says that most people who were aware of the program did not know it was being offered to public patients in Canberra.
‘They were delighted to have the opportunity to access it for their public patients.
'And the patients loved it. The patients we interviewed who had done GLA:D said, “Why didn’t my GP tell me about this?” They found that doing exercise with GLA:D was so much better for them than trying to join their local gym, where they often felt out of place and sometimes felt unsafe.
'They felt a sense of community with the other people in the program and they knew they were being looked after professionally.
'Patients were very happy with GLA:D and GPs have been very happy with it too.’
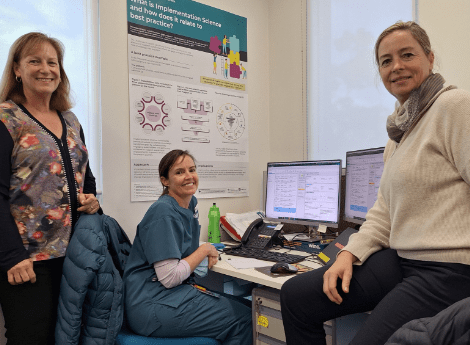
The Canberra Health Services team: Jennie Scarvell, Professor of Physiotherapy University of Canberra; Deb O’Kane, advanced practice physiotherapist orthopaedics; and Danealle Gilfillan, advanced practice physiotherapist.
While the results of the research project are still being evaluated, Jennie says the initial indications are that there has been a reduction in the number of patients on the waiting list and that the wait times for those patients proceeding to surgery are much shorter.
Potential cost savings to be made by directing patients through a conservative management pathway have also yet to be finalised but look promising.
‘There’s been high satisfaction with physiotherapist screening among people on the waiting list,’ Jennie says.
‘We can’t give you the cost savings yet but we can tell you that a whole lot of people have been moved over to non-surgical management.
'A lot of people don’t want to have a knee replacement but don’t know that there is any other way.
'Our public people are actually coming off the surgical waiting lists.’
Jennie says that the waiting time for Category 2 patients was previously sitting at a mean of 200 days, while Category 3 patients waited for a mean of 800 days.
Category 2 patients now wait 131 fewer days and Category 3 patients spend a whopping 793 days less waiting time before joining the official waitlist.
‘This is because they’re all getting screened now.
'If they are Category 3 patients, they shouldn’t be having a knee replacement anyway because they’re not severe enough.
'Category 3 means they’re not urgent. All these people get physiotherapy in the community now,’ Jennie says.
‘Category 2 people will see a surgeon.
'They’re getting screened and then they’re seeing a surgeon but they’re seeing the surgeon within 2.5 to three months now whereas previously they were waiting nearly a year.’
A physiotherapist in Canberra and Canada for 15 years, Jennie has previously worked at Canberra Hospital and in 2004 she completed her PhD, entitled ‘Kinematics and degenerative change in ligament-injured knees’.
She helped to roll out the Bachelor of Physiotherapy program at UC and has experience in rheumatology, orthopaedics and hydrotherapy.
Over the course of her career, Jennie has worn the various hats of physiotherapy clinician, academic and researcher and has developed a keen interest in knee motion in injury, total joint replacement, outcomes from surgery and rehabilitation, prevention and treatment of fractures, and medical imaging—particularly 4D modelling.
Jennie says this current research project was conducted partly to correct misinformation in the community about knees and OA.
Leaving myths about knee OA unchallenged can be dangerous because it allows ideas to proliferate that can hinder effective management and treatment of the condition.
For example, a belief that exercise exacerbates the disease can lead patients to avoid physical activity, worsening their symptoms and overall joint health.
Myths about the inevitability of severe pain or a sole reliance on surgery can prevent individuals from exploring beneficial non-surgical treatments such as physiotherapy.
Because misinformation can result in delayed diagnosis, inappropriate self- treatment and reduced quality of life, it’s crucial to challenge it and to ensure that patients receive accurate information, enabling them to make informed decisions about their health and treatment options.
‘In the public chatter, you hear things like “My knee has worn out. I need a new one.”
'But it’s not a fridge.
'It’s not a tyre or a machine.
'Knees will actually respond very well to exercise, unlike tyres, which get worn out,’ Jennie says.
‘Most of us are going to take our knees with us when we go; we’ve just got to learn how to manage them.
'There are people who do need a knee replacement and the right person will do really well with a knee replacement at the right time.
'But they’re all going to get a better knee outcome if they do GLA:D first.’
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.





