Direct access to physio reduces GP strain in Norway

A recent study by Australian and Norwegian researchers explored the impact of a direct-access physiotherapy model for musculoskeletal conditions on the Norwegian health system.
Until 2018, if Norwegians wanted to see a physiotherapist, they had to first obtain a referral from a GP.
Legislative change did away with this step and now this population can access physiotherapy services directly.
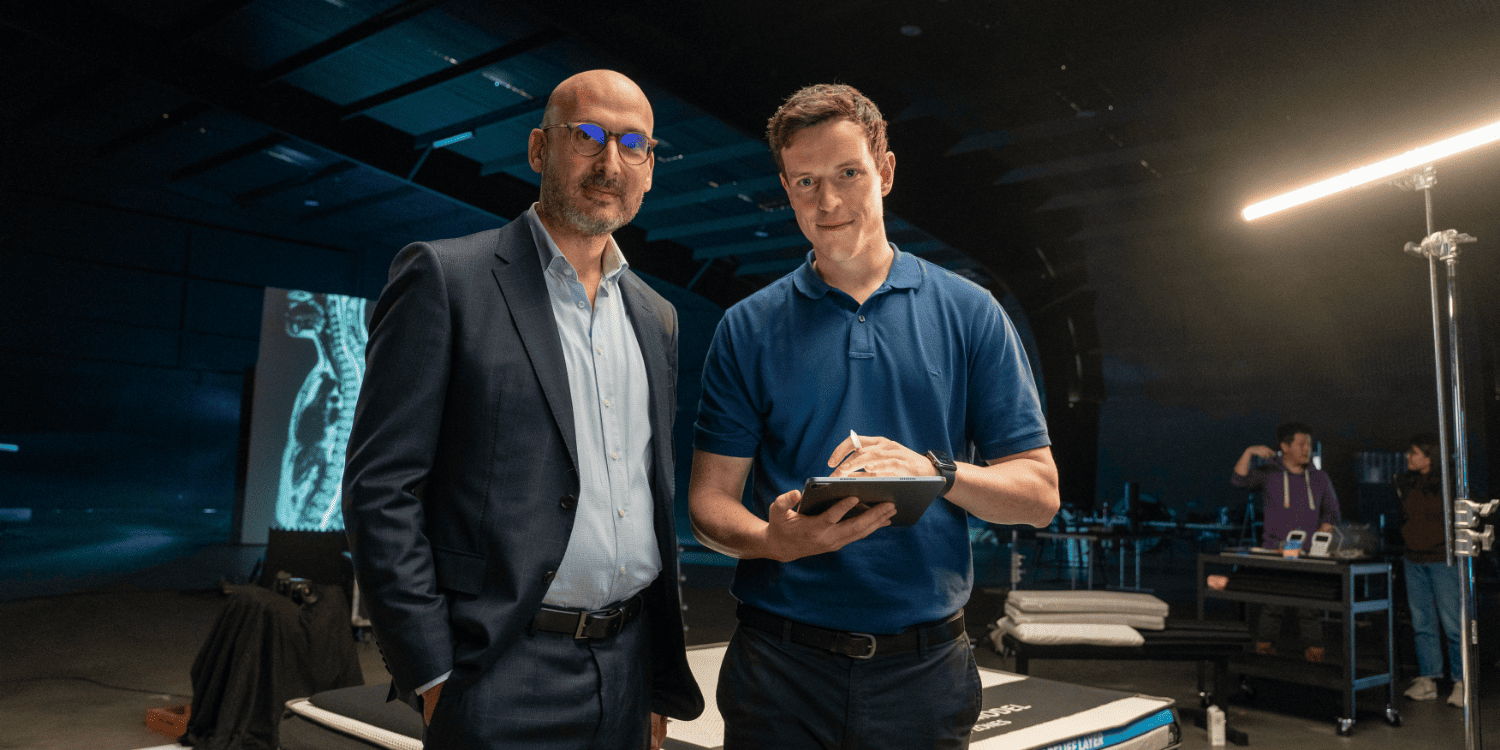
Jim Zouch APAM, a physiotherapist and PhD candidate in the Faculty of Medicine and Health at the University of Sydney, was one of a team of researchers interested in studying the effect of the law change on rates of primary and secondary care consultations for musculoskeletal (MSK) conditions in Norway.
This project was the third study completed as part of his PhD.
‘The research looked at the impact of the initial provider on outcomes for patients with musculoskeletal pain,’ says Jim.
‘In Norway they have access to very accurate data about primary care because there are diagnostic codes for every consultation.
'We thus had a perfect opportunity to look at how a direct-access physiotherapy model works and at its impact on the Norwegian healthcare system.’
The study looked at data from 82,072 participants, which was derived from three sources: the HUNT4 Survey (here), conducted 2017–19 (n=56,038); the Tromsø7 survey (here), conducted 2015–16 (n=21,068); and the Musculoskeletal pain in Ullensaker Study (here), conducted 2010–11(n=4966).
Using an interrupted time-series design, the data was analysed for a pre-intervention period of 2014–17 and a post-intervention period
of 2018–21.
The study examined two primary outcomes: the rate per 10,000 participants of GP and physiotherapy consultations for MSK conditions in primary care and the rate per 10,000 participants of specialist consultations (eg, consultations with rheumatologists, pain specialists or
rehabilitation physicians) and surgical procedures for back and neck conditions.
Secondary outcomes looked at the influence of age, education level and MSK diagnosis on the rates of consultations.
Previous research had shown that older patients may be reluctant to directly access physiotherapy services due to the perceived complexity of their condition or the presence of comorbidities.
Research had also demonstrated an association between higher education levels and increased use of specialist healthcare, reflected in higher uptakes of self-referral for physiotherapy services.
MSK conditions were categorised into shoulder, neck, knee and back pain.
‘We found that almost immediately after the introduction of this national policy in Norway, where patients could go directly to a physio, there was a 10 per cent reduction in the number of people going to see their GP for a MSK complaint,’ says Jim.
‘But the rates of physiotherapists’ consultations remained the same, which might sound confusing.
'What we believe happened was that some patients, who would previously have gone to see their GP first before seeing a physiotherapist,
simply skipped that step and went straight to the physiotherapist.
‘There is only a small number of physiotherapists with contracts to deliver publicly funded access in Norway.
'The impact on GP consultations may have been greater if there was more availability of physiotherapists.’
In regards to the primary and secondary outcomes, there was no increase in the rates of specialist consultations or surgery for spinal conditions.
There was a reduction in the rates of physiotherapy MSK consultations for people with lower levels of education following the introduction
of the direct-access model as well as a reduction in spinal operations in people aged between 40 and 60, six months after the model’s introduction.
The researchers did not observe any association between the model’s introduction and the rates of consultation for different MSK conditions
(back, neck, shoulder and knee).
Strengths of the study include the longitudinal analysis of routinely collected health data from a large patient sample, showing broad representation of the Norwegian population.
Limitations relate to the lack of patient-level data, preventing strong conclusions explaining healthcare utilisation rates associated with the direct-access model of care, and to the reliability of the results, due to variability in the GP regression model following the
introduction of measures to help control the spread of COVID-19 in 2020.
The applicability of results to countries classified as middle or low income may be difficult due to the high-income status of Norway and its well-established healthcare system and mixed-payment model.
What does this research mean for Australia?
‘We know that in Australia, 20–25 per cent of a GP’s case load is made up of people with MSK consultations so it’s a big chunk of time,’ says Jim.
‘We have a huge workforce of physiotherapists who can offer this care and we know that it’s safe.
'But we need to examine these models in Australia before we can understand what it means for us, such as with piloted trials of publicly
funded physios.
‘It would also be interesting to explore in future research how the starting point affects a patient’s outcome—that is, whether seeing a GP first or a physiotherapist first influences their care in terms of waiting time, imaging, sick leave and other factors.
‘This was a very collaborative project, with fantastic support from OsloMet University in Norway in regards to their healthcare
system, database and local knowledge.
'I’d also like to thank Paulo Ferreira, my supervisor, as well as the University of Sydney for its ongoing support.’
Reference: Zouch J et al. Reducing strain on primary healthcare systems through innovative models of care: the impact of direct access physiotherapy for musculoskeletal conditions—an interrupted time series analysis. Family Medicine and Community Health. 2024;12(3):e002998. doi: 10.1136/fmch-2024-002998
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.