Identifying cause of hip pain is key
With more than 30 years’ experience as a clinical practitioner, Dr Angela Fearon will present a new course entitled ‘A pragmatic approach to lateral hip pain’ on 24–25 May.
What can participants expect from this new PD offering?
Do you remember the light bulb moment when you understood how gluteus medius on the stance leg held up the pelvis during gait? For me it was in the same week I remember seeing a video of someone walking pre- (with a marked Trendelenburg gait) and post- (with no Trendelenburg gait) total hip replacement. I have been fascinated about the relationship of hip pain, and gluteus medius function to gait ever since.
Over the past 12 years I have been researching hip pain in older people. My research (and that of others) has informed my clinical practice, and my clinical practice has informed my research. I want to share my research and clinical insights into hip assessment, treatment and management strategies with other physiotherapists. Because the course focuses on gluteal tendinopathy, we’ll cover how to treat tendons in general, along with the specifics for gluteus medius tendinopathy. Participants will also learn about a taping technique that has some good evidence to support its use.
What are some of the traps in trying to identify the correct cause of hip pain?
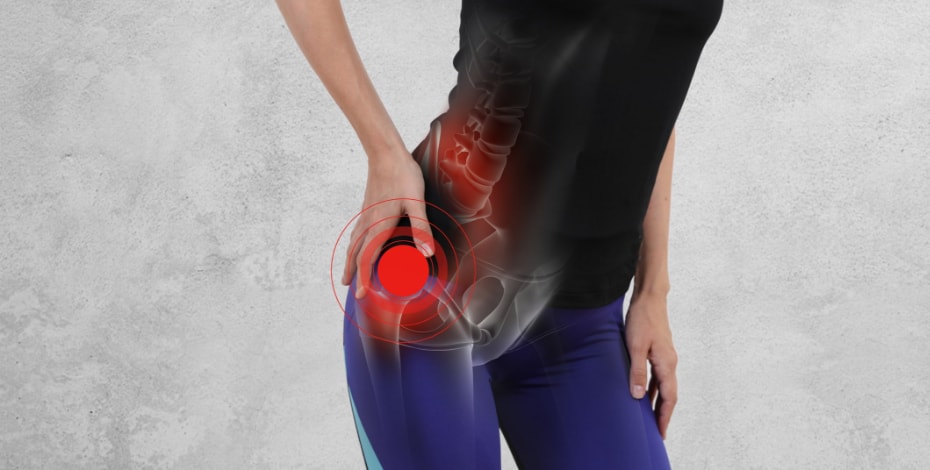
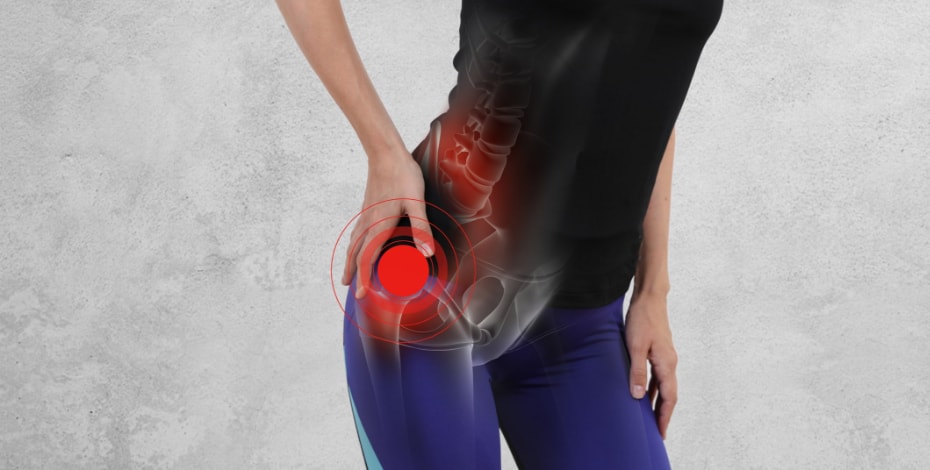
When patients come in to see me, they frequently tell me they have ‘hip pain’. They then point to their greater trochanter, sacroiliac joints or even their back. Thus, identifying what the patient means by ‘hip pain’ is really important. That established, identifying the underlying cause of the pain can be tricky because lateral hip pain can be secondary to lumbar spine or hip joint referral, or the over tissues. There are also lots of muscles around the hip, so differentiating these (eg, between quadratus femoris and gluteal tendinopathy) can be tricky.
Teasing out the cause of pain can generally be done clinically when you know the right tests and how much weight to put on the results. A further important aspect of assessment and management is identifying the co-morbidities that a person has—and dealing with these confounding conditions.
Finally, physiotherapists need a good understanding of the effects of pain, placebo and nocebo. We need to be aware of how much we can help someone who is in pain by reassuring them (when appropriate) and not scaring them (which is never appropriate). For example, many patients will present with imaging that states that they have a tendinopathy or even a ‘tendon tear’. Clinicians know that this may, or may not, be the underlying cause of the patient’s pain.
Plenty of people have completely pain-free tendinopathy and even tears around the hip (Docking et al 2019 inpress). We need to take this into account when assessing someone. We know that good physical rehabilitation and appropriate advice is likely to help the majority of people with hip tendinopathy (Mellor et al 2018, Ganderton et al 2018).
Who will benefit most from attending the course?
Anyone who finds treating older people with hip pain a challenge, physiotherapists who are interested in new ideas or would like to get together and share ideas. All are welcome.
This is a friendly and non-judgemental environment in which I meet lots of people and share my knowledge and clinical experience with them, and them with me. This course isn’t designed for managing younger people with sports-related hip pain.
A pragmatic approach to lateral hip pain
24–25 May 2019
Orange, New South Wales
Click here to register.
Dr Angela Fearon, APAM, is a lecturer and researcher in physiotherapy at the University of Canberra. Angie has presented her research findings around lateral hip pain locally and internationally and has more than 30 years of clinical practice experience
© Copyright 2024 by Australian Physiotherapy Association. All rights reserved.





