New clinical recommendations for whiplash
Professor Trudy Rebbeck, Dr Christopher Papic and Professor Michele Sterling consider new clinical recommendations for whiplash management and their impact on physiotherapy practice.
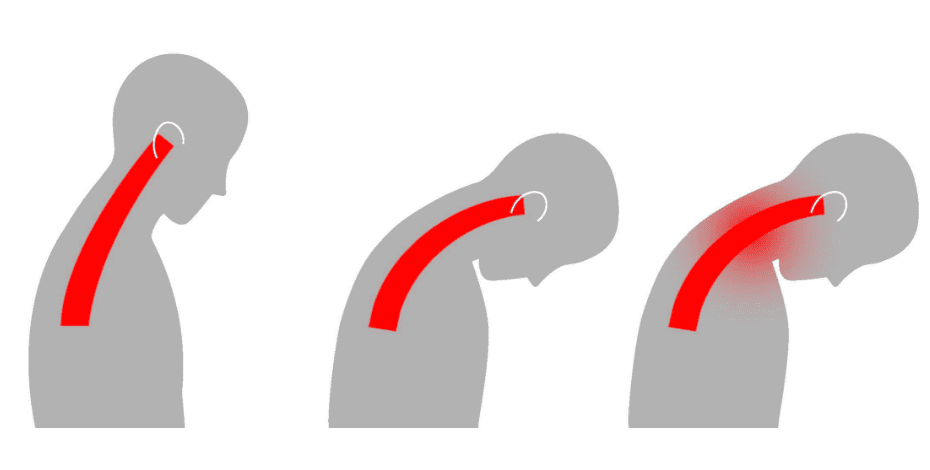
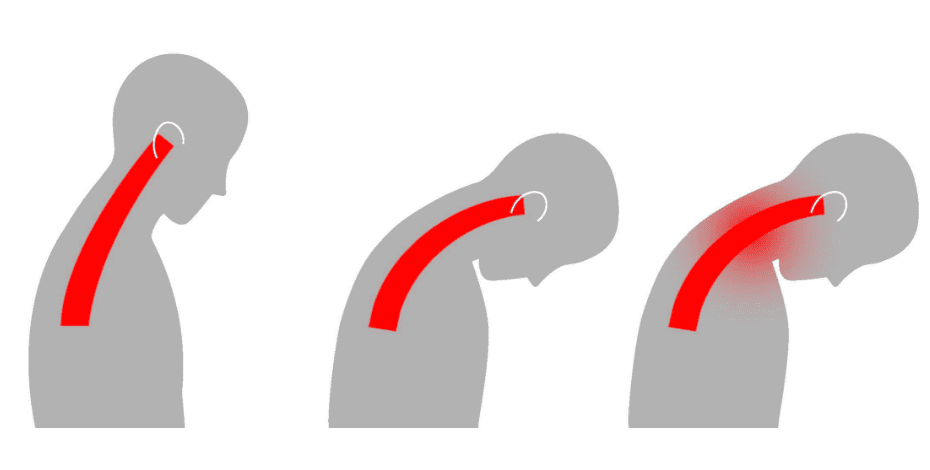
Whiplash associated disorders (WAD) are the most common injuries sustained in motor vehicle crashes.
While half of Australians recover rapidly after whiplash injury, the other half may develop long-term pain, disability and psychological distress that interferes with daily life.
This poor recovery rate is reflected in the $1 billion of annual costs associated with rehabilitation and management of whiplash in Australia.
Three iterations of clinical guidelines for whiplash have been developed and implemented over 20 years in Australia.
Australian physiotherapists have demonstrated excellent uptake of some recommendations (eg, to provide advice and exercise) but rarely assess for prognostic risk or change care based on prognostic risk status (Griffin et al 2019).
Referral pathways for people who don’t recover continue to involve numerous, often unnecessary imaging and/or inappropriate referrals to surgeons (Bandong et al 2018).
New clinical recommendations for whiplash
New clinical recommendations for whiplash developed by researchers and clinicians at the University of Sydney will underpin future Australian clinical guidelines.
The recommendations were developed to provide clinicians with an updated evidence base for the assessment, prognosis and treatment of whiplash.
The recommendations were informed by a series and were developed following the GRADE (Grading of Recommendations Assessment, Development and Evaluation) process and evidence-to-decision framework.
This framework allows researchers to consider the balance between benefits/harms, cost, equity, acceptability and feasibility of assessment methods and treatment interventions when developing recommendations.
What are the key recommendations for Australian physiotherapists?

Professor Trudy Rebbeck, from the University of Sydney, is involved with the development of the guidelines as well as the My Whiplash Navigator website.
Clinical recommendations rarely implement themselves.
Determining key recommendations for implementation based on gaps in current practice assists with likely translation into clinical practice.
Key recommendations for people with acute whiplash
Diagnosis—use the Quebec Task Force classification system to classify whiplash from grade 0 to grade IV.
The Canadian C-spine rule should be used to screen for cervical fracture (WAD IV), neurological assessments to determine cervical radiculopathy (WAD III) and cervical range of motion and palpation to classify WAD I–II.
Advanced imaging should be reserved for patients with suspected cervical radiculopathy who are not showing improvement with treatment and should not be used for patients with pain and musculoskeletal signs only (grade II).
Prognosis—assess for risk of poor recovery using a validated tool, either WhipPredict (Sterling et al 2021) or the Short Form Örebro Musculoskeletal Pain Screening Questionnaire (Linton et al 2011).
Assessment—a standard assessment of symptoms (eg, pain severity, disability) and a basic physical examination (neurological, cervical range of motion) should take place in all patients with whiplash.
Additional assessment of other domains such as muscle performance and function, sensorimotor control, sensory sensitivity and psychological distress (eg, post-traumatic stress) should be reserved for patients at medium/high risk of poor recovery.
The results of these assessments can be used to guide treatment.
Reassessment of pain (using the Numeric Rating Scale) and neck- related disability (using the Neck Disability Index) should be done at regular intervals to evaluate whether the patient is responding to the treatment.
Treatment—frontline treatment recommendations include providing accurate advice, neck-specific exercises and simple medications (eg, simple analgesics).
Specific exercises for dizziness and psychological strategies are recommended for those at medium/high risk of poor recovery.
Other treatments such as multimodal physical therapy or stronger medication may be considered in certain cases in addition to recommended care.
Surgery and injections are not recommended.
Referral—referral to whiplash specialists is recommended for those at medium/high risk who are not recovering well, as an alternative to the current pathway.
Whiplash specialists are clinicians with advanced expertise in whiplash, most commonly Specialist Musculoskeletal Physiotherapists or Specialist Pain Physiotherapists (as awarded by the Australian College of Physiotherapists).
Key recommendations for people with chronic whiplash
Assessment—reassess the whiplash grade during the chronic phase, along with assessment of neck pain, self-reported disability and psychological health (eg, depression, post- traumatic stress symptoms and perceived injustice), to identify individuals likely to experience ongoing pain and disability.
If indicated, other assessments can be carried out such as sensory sensitivity (eg, cold allodynia), cervical muscle and sensorimotor assessments.
Treatment—similar to acute whiplash, advice and neck-specific exercises are recommended.
However, advice should differ from the acute phase, with greater emphasis on how psychological distress can influence pain and physical function and on strategies for self-management of chronic pain.
Dizziness-specific exercises are recommended for those experiencing dizziness, such as oculomotor control and balance exercises as indicated through appropriate assessment.
People at medium/high risk of poor outcome may benefit from exercise combined with psychological strategies that target stress and pain.
Referral—multidisciplinary care should be considered for patients who present with pain and with physical and psychological distress and who have not responded to recommended treatments.
This may include trauma-focused cognitive behaviour therapy delivered by a psychologist after appropriate assessment.
Once again, referral to whiplash specialists should be considered if it has not occurred to date.
Implementation: My Whiplash Navigator and beyond

Dr Chris Papic is an exercise physiologist and researcher at the University of Queensland who helped to develop the guidelines and website.
Physiotherapists will be critical to ensuring effective implementation of these recommendations.
They are among the most commonly consulted healthcare professionals for people with whiplash injury and many of the clinical recommendations fall within the scope of practice of physiotherapists.
To assist with implementation, Trudy, Michele and colleagues have developed a series of resources and guides through My Whiplash Navigator, which was co-designed by clinicians, people with whiplash, researchers and government regulators (Bandong et al 2019).
Assess for prognostic risk
The WhipPredict screening tool (tinyurl.com/T0N6M9R) should be completed by day 7 post-injury to classify the risk of poor recovery and to determine the next steps.
The tool can be completed by patients online on My Whiplash Navigator.
The downloadable results include appropriate messaging to the patient about what their risk classification means.
Don’t over-complicate care for people at low risk
People screened at low risk (of poor outcome) will recover well with minimal intervention (on average three sessions) and therefore shouldn’t be overtreated because this may complicate recovery.
Physiotherapists can advise people about a good recovery, how to return to usual activities and how to remain active.
Neck-specific exercises may be prescribed.
My Whiplash Navigator can be used to reinforce these messages and has links to videos for patients on how to perform the exercises.
Take the next steps for medium/high risk patients
Assess additional domains
For patients who are not recovering after the initial recommended treatment (advice and neck-specific exercise), physiotherapists should consider additional physical and psychological assessments.
My Whiplash Navigator contains links with practical guides on how to assess these domains.
Provide psychological strategies that target stress and pain
Early post-traumatic stress symptoms are associated with ongoing pain and disability and are a predominant feature of people at medium to high risk of poor recovery.
To implement psychological strategies, physiotherapists may need to upskill.
StressModex (stress inoculation training plus exercise) is an intervention that integrates simple psychological strategies into physiotherapy to target early stress symptoms.
It is delivered by physiotherapists to people with acute whiplash at risk of poor recovery.
In a randomised clinical trial, it resulted in clinically relevant improvements in pain-related disability when compared to physiotherapy alone (Sterling et al 2019).
A secondary analysis showed that effects on disability were exerted through reducing stress symptoms (Elphinston et al 2020), demonstrating that physiotherapists can successfully improve patients’ stress levels and enhance recovery for people with acute whiplash.
Physiotherapists can access the StressModex training modules through My Whiplash Navigator.
Or refer to a whiplash specialist
If a physiotherapist is not confident about implementing simple psychological strategies or conducting a more comprehensive clinical assessment of a patient’s impairments, then the patient should be referred to a whiplash specialist (often a specialist musculoskeletal or pain physiotherapist).
Specialist physiotherapists then undertake a comprehensive assessment of the additional assessment domains before collaboratively (with the patient and the primary care physiotherapist) recommending future care pathways such as:
- shared care—management of the patient by the primary healthcare professional, with guidance
- specialist-led care—a short course of specialist-led care (up to six sessions) when the primary healthcare professional is less confident (eg, not confident about managing complex symptoms such as dizziness or headache)
- referred care—facilitated multidisciplinary care, (eg, with a psychologist or a pain physician).
This model of care is well tested and accepted by both patients (Beales et al 2024) and clinicians (Bandong et al 2019, Kang et al 2022).
It was recently evaluated in a randomised controlled trial without improving the primary outcome (disability) but with a small positive effect on pain self-efficacy (Rebbeck et al 2023), leading to the cautious recommended collaborative approaches taken here.
What about chronic whiplash?
When managing patients with chronic whiplash, the focus is on active physical therapy with an emphasis on developing self-efficacy and providing psychological support when indicated.
If the patient does report elevated levels of psychological distress, the physiotherapist should consider referral to a mental healthcare professional.
Multidisciplinary care is more likely during this phase of whiplash and it is important for physiotherapists to maintain appropriate interdisciplinary communication to ensure that care is coordinated for the patient.
Find out more

The University of Queensland's Professor Michele Sterling is leading a trial to scale up and implement training for the StressModex treatment. .
Free online resources and associated evaluation studies are now available.
My Whiplash Navigator is a website developed by the University of Sydney and the University of Queensland in conjunction with the New South Wales State Insurance Regulatory Authority and the Queensland Motor Accident Insurance Commission.
The website now includes bespoke resources developed by people with whiplash, clinicians and insurers.
Visit the website for more information.
Three interactive whiplash case studies feature people with different prognostic risk profiles.
Clinicians can work through these cases with the aim of consolidating their clinical reasoning with respect to assessment, prognosis and management.
The case studies are embedded within student and postgraduate education opportunities (eg, APA advanced cervical spine courses).
You can also be part of research evaluating the usefulness of both the website and the case studies by completing the consent forms on the website or by contacting the authors.
Sign into My Whiplash Navigator as a healthcare professional and visit the Interactive Learning Hub to find out more.
In a current trial funded by the Medical Research Future Fund, we are working on implementing and scaling up training in the StressModex treatment for physiotherapists.
Participants will be randomised to receive either online training over six weeks or face-to-face training over two days.
In both cases, training will be delivered by a clinical psychologist and an expert physiotherapist.
Contact Michele if you are interested in participating in this trial.
Whiplash and other traumatic musculoskeletal conditions can be difficult to manage.
This combined work of developing clinical recommendations, resources and training packages aims to assist physiotherapists to gain the skills to manage people with whiplash effectively and confidently.
>> To engage in these projects and future implementation research in this area, contact Trudy at trudy.rebbeck@sydney.edu.au, Michele at m.sterling@uq.edu.au, Chris at c.papic@uq.edu.au and Dr Ana Paula Carvalho- e-Silva at ana.carvalhosilva@sydney.edu.au.
>> Professor Trudy Rebbeck FACP is a clinician–researcher and educator. Trudy is Professor of Clinical Translation in Allied Health at the University of Sydney and a Specialist Musculoskeletal Physiotherapist (as awarded by the Australian College of Physiotherapists in 2007).
>> Professor Michele Sterling FACP is a NHMRC Leadership Fellow (L2), program lead at RECOVER Injury Research Centre and director of the NHMRC Centre of Research Excellence in Better Health Outcomes for Compensable Injury, both at the University of Queensland. Michele is a Research Fellow (Fellow by Original Contribution) of the Australian College
of Physiotherapists.
>> Dr Chris Papic is a research fellow in musculoskeletal injury at RECOVER Injury Research Centre at the University of Queensland and a lecturer in clinical exercise physiology at the University
of New England, with a focus on musculoskeletal rehabilitation. Chris has ten years’ experience as a clinical exercise physiologist in a rehabilitation hospital.
Quick links:
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





