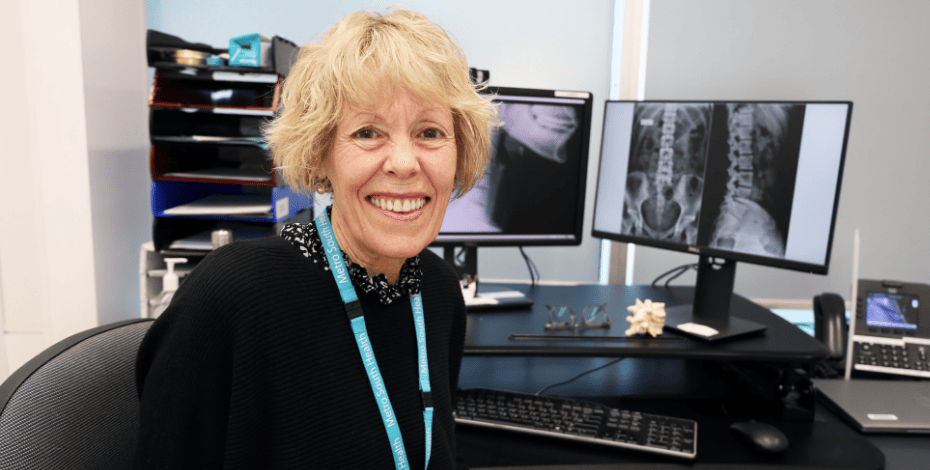
The long road to advanced scope physiotherapy
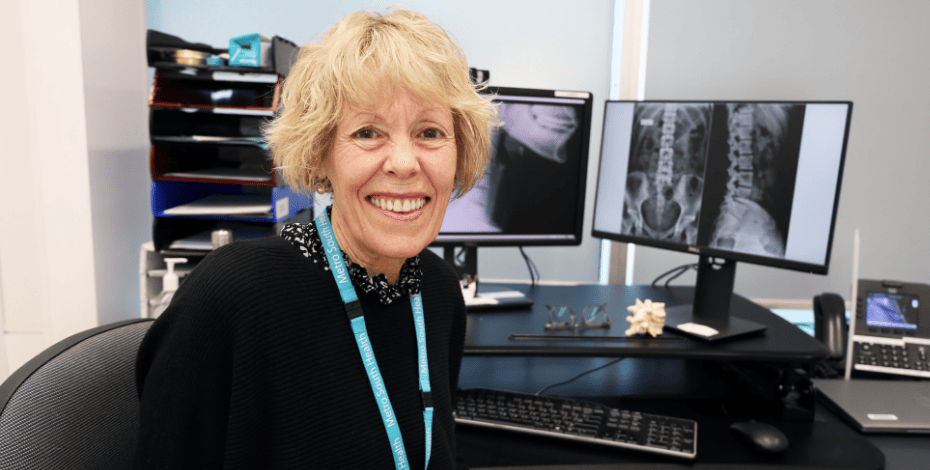
Having been at the forefront of introducing advanced scope physiotherapy to the Princess Alexandra Hospital in Brisbane, Erica Williams reflects on the challenges she and the team faced, including scepticism from medical professionals and initial doubts about their suitability for the role.
Knowing the depth and breadth of your skills and capabilities as a physiotherapist is one thing. Convincing others can be
an entirely different matter.
For Dr Erica Williams FACP, one of the biggest hurdles to overcome when advanced scope physiotherapy was first trialled at Princess Alexandra Hospital in Brisbane in early 2006 was convincing surgeons and general practitioners that she and colleagues on her team were up to the task.
Attending her first meeting with the hospital’s orthopaedic team about the rollout of the then-12-month pilot project, which was part of the early establishment of the orthopaedic physiotherapy screening clinics in Brisbane, Erica expected to simply be introduced.
However, she soon found herself being quizzed about her skills, knowledge and capabilities for the role.
The primary concerns of those in the room, Erica says, centred on whether advanced scope physiotherapists would identify red flag presentations, whether they had the requisite knowledge and experience to determine a patient’s suitability for review by the surgeons and whether they might potentially miss something critical during assessment.
Erica, a Specialist Musculoskeletal Physiotherapist (as awarded by the Australian College of Physiotherapists in 2008), and her physiotherapist colleagues Luen Pearce and Sheryl Pahor had been invited to triage patients on the spinal orthopaedic waitlist, which at the time was very long; some patients had been waiting up to five years to see a surgeon.
The advanced scope physiotherapy team was to help manage the spinal orthopaedic waitlist—directing patients considered suitable for conservative management to the multidisciplinary team, which included physiotherapists, while sending others on for consultation with surgeons.
All of this work was done in collaboration with the spinal surgeons, allowing the advanced scope physiotherapists to showcase their skills as well as open themselves up to peer supervision, revision and critique.
Each patient on the orthopaedic waitlist was reviewed and every case presentation was different.
Given that each surgeon also worked differently and preferred different imaging, there was a lot for the advanced scope physiotherapists to consider in their determination of which treatment pathway was suitable for each patient.
On top of that, many of the GPs who had referred patients to see a surgeon were dubious about their patients being triaged and managed by an advanced scope physiotherapist.
‘There was a lot of scepticism as to whether or not we could actually do it,’ Erica says.
‘Some of the surgeons didn’t think we were up to deciding who was appropriate for surgeon review and who wasn’t.
'And that was a steep learning curve for us. It really was.
'But we also had the support of a few surgeons who were very willing to share their knowledge and those relationships were vital to the success of the project.
‘Initially there was resistance from the GPs, a lot of resistance. They’d say “I sent them to see a surgeon; why are they seeing a physio?”’ Erica says.
‘We did a lot of PR with the GPs and part of that was writing concise but comprehensive letters back to show them that we knew what we were talking about.
'And then they started saying “Oh, okay, they [patients] have access to a multidisciplinary team.” There were lots of barriers, mostly related to the thought that we couldn’t do the job.
'There was, and still is, a lack of understanding of higher education in physiotherapy.
'We continue to write letters to the GP every time we see a patient, whether it’s an initial consult or a follow-up.
‘We also had resistance from patients who thought they would be seeing a surgeon.
'However, there were very few who were still unhappy by the end of the consultation because we had time to explain their problems to them and why a particular pathway was appropriate—explanations that surgeons generally don’t provide when dealing with non-surgical patients.’
Advanced practice physiotherapists have high levels of clinical expertise and experience, allowing them to assess and independently manage a specific cohort of patients, often with complex presentations.
In addition to general physiotherapy skills, advanced scope physiotherapists have attained a higher level of education, usually a master’s degree, and have consolidated that knowledge with a few more years of practice afterwards.
They need to be open to learning, Erica says, and to be able to work cohesively and collaboratively with other medical professionals.
Advanced scope physiotherapists are also advocates for their own high level of skills and abilities, sharing knowledge and experience more broadly.
The process of educating others about advanced scope physiotherapists’ skills and expertise was slow going at first, Erica says.
While the advanced scope physiotherapy team was addressing the clinical hurdles, three physiotherapists heading up the orthopaedics team—Brett Baxter, Peter Tonks and Louise Matthews— did a lot of communication with the hospital stakeholders to get the service established.
Overcoming initial resistance, the physiotherapists slowly dismantled the barriers and began getting runs on the board.
With the numbers on the spinal orthopaedic waitlist reducing thanks to the physiotherapy-led clinic and the multidisciplinary model of care at Princess Alexandra Hospital, the team was then given another challenge to tackle—the hospital’s longer neurosurgical waitlist.

Erica Williams (centre) with advanced scope physiotherapy team members Jody Anning, Louise Matthews, James Farmer and Jennie Wong.
‘Our role was to work out which patients actually needed to see the surgeons and which patients weren’t appropriate for surgery because the surgeons were spending so much of their time in clinic seeing patients who didn’t need surgery,’ Erica says.
‘Our model of care was comprehensive. We had the multidisciplinary team so we could refer patients there.
'We could then reassess them and discharge them, with almost 70 per cent not requiring review by the surgeons.
'We could also escalate care for patients who needed to see a surgeon urgently.
‘There were a lot of patients who were on both the neurosurgery and the spinal orthopaedic waitlists for the same condition. That was a problem because it blew out figures on both waitlists.
'As a result, the hospital combined spinal neurosurgery and spinal orthopaedic surgery and created the Spinal Surgical Service.’
The hospital’s Back Assessment Clinic and Multidisciplinary Service, where Erica has been employed as a specialist physiotherapist since 2006, receives GP-referred patients who have been first triaged as category 2 or 3 by the Spinal Surgical Service.
Of these patients, only 14 per cent proceed to surgery and the remaining 86 per cent are managed non-surgically.
Rather than being redirected back to their GP, these patients have the opportunity to access specialised spinal pain treatment from a multidisciplinary service.
Recalling those early days of the advanced scope physiotherapy rollout, Erica says that after their success in reducing patients on the spinal orthopaedic and neurosurgical waitlists, Erica and Sheryl were approached to look at the spinal surgery waitlist—that is, the patients who had seen the surgeons and been deemed appropriate for surgery but at that time were waiting significant periods of time for their surgery to be scheduled.
Such was the level of trust in the abilities of these advanced scope physiotherapists by then that they were asked to reassess the patients for the surgeons.
‘We went through the whole of that category 2 waitlist for surgery to see whether each patient was still alive, whether they had other medical issues that would preclude them from surgery and so on.
'The aim was either to take them off the waitlist (which we were able to do independently if we thought it was okay) or, if we thought they still needed surgery, to get them in, review them and update their imaging before getting them back in to see the surgeons,’ Erica says.
Another advantage of the early assessment of patients through these clinics has been the not-infrequent identification by the advanced scope physiotherapists of serious pathology that had been overlooked, with subsequent escalation of care.
Erica recalls one patient who was referred by her GP to the Spinal Surgical Service, triaged to Erica’s clinic and, following imaging, discovered to have multiple sclerosis.
Erica was able to have the imaging reviewed by the neurosurgeon and then by a neurologist and to have the patient in hospital for infusion therapy that afternoon.
A major expansion of the advanced scope physiotherapy service at Princess Alexandra Hospital took place in 2016 when additional staff were added.
Erica says the team has gone from strength to strength since then.
‘Our team is great now. We are all so eager to learn from each other and to learn about difficult patients and we’re happy to discuss everything and to be open to critique,’ Erica says.
‘You need to have that attitude when you come into this service—not only to be part of the team of the physio clinical leads but also to be part of the team with the surgeons.
'The surgeons are now very supportive of our clinic and its success has had a lot to do with relationship building.
‘Another aspect is mentoring the multidisciplinary team. We do quite a lot of mentoring of the younger physios who come into the multidisciplinary team and we also encourage them to go off and do their master’s degrees.
'And, of course, the most rewarding aspect of the service is that we provide a great patient pathway with timely and appropriate management for patients referred to the Spinal Surgical Service.’
© Copyright 2025 by Australian Physiotherapy Association. All rights reserved.





