Future of Physiotherapy in Australia: A 10-Year Vision Policy White Paper
The APA’s white paper sets out a transformative reform path. We outline new opportunities that leverage the physiotherapy workforce to support healthier lives and drive system-level change to advance health, improve care and increase value.
Launched at FOCUS2022, the white paper has already received the support of Minister for Health and Aged Care, the Hon. Mark Butler MP via a video recording to open the conference. It outlines a clear vision on the reform of the health system and the vital role of physiotherapy.
From vision to action
Physiotherapy will be key to putting high-value care to action in Australia.
In forging a realistic path to healthcare reform in Australia, we have set solutions to connect and integrate care to deliver the four outcomes governments and patients want—high-value care, reduced costs, improved efficiency and giving patients enhanced ownership of their own healthcare.
We encourage all members to get behind our vision and participate in the policy discussion to ensure a strong voice for physiotherapy in reform.
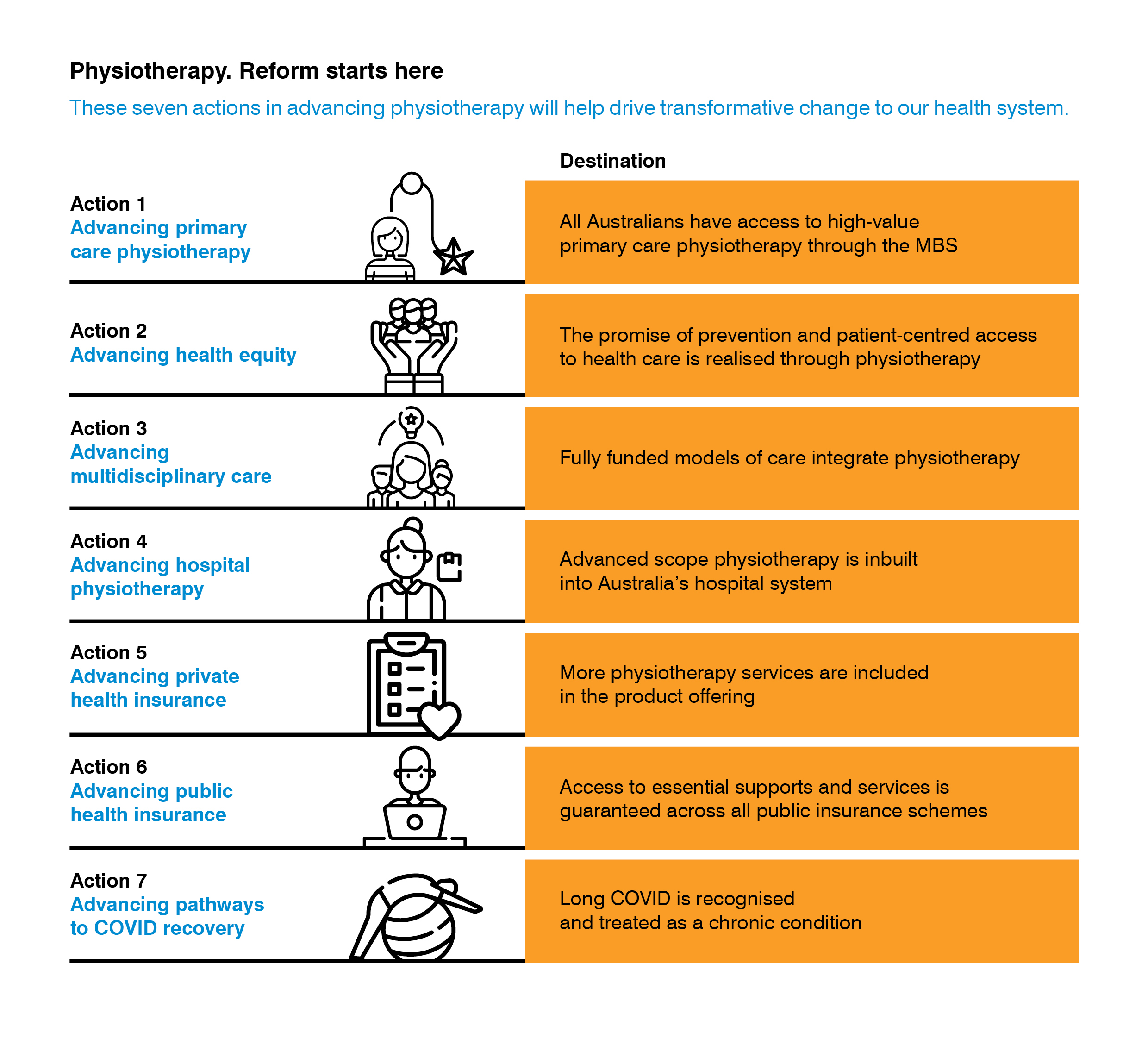
The APA’s solution for reform is presented in seven detailed actions.
The paper, written for a funder audience, envisions a policy roadmap that, if implemented, would advance health, strengthen care and increase value. This comes at a critical moment in the reform process which provides a new policy window to ensure an expanded role for physiotherapy in the healthcare system.
We offer fresh solutions to healthcare reform and outline physiotherapy-led models to strengthen care and health outcomes, reduce disparities across priority populations, and bring efficiencies to the health system.
A framework for action
Our vision is to ensure that all Australians have access to publicly funded physiotherapy.
We outline a path to better care that optimises the patient journey by removing current structural barriers and investing more in public physiotherapy.
We call for renewal of the Medicare system through investment in publicly funded First Contact Physiotherapy in primary care. We also call for better access to chronic disease and pain items and for the expansion of preventive and restorative healthcare through new physiotherapy-led models.
At the heart of the changes is restoring fairness to achieve more equitable health outcomes for priority population groups.
We set the fair foundations we need for health equity and access. The first step involves gaining access to affordable healthcare. There’s a two-speed health system—those who can cover their health costs with their own money and those who can’t. It doesn’t have to be that way.
The shift from reactive models to preventive healthcare is essential. We need to pick up the pace through the accelerated establishment of new preventive healthcare models across priority populations who are the most at risk of poor health outcomes. It is these priority populations, including Aboriginal and Torres Strait Islander peoples, people from a low socio-economic background, culturally and linguistically diverse populations, people living in remote areas and people living with disability, that stand to benefit the most from physiotherapy-led prevention.
The most fundamental reform will provide a way forward to overcome the barriers to team-based care.
We outline new approaches to funding team-based care in order to deliver the best health and system outcomes. This remains a central reform challenge in Australia. For integration to be successful, a commitment to funding greater access to physiotherapy and multidisciplinary care that encompasses the entire health workforce is vital.
Fully funded and integrated models are needed across the health system, with a focus on aged care and cancer care and on formalising funding between physical and mental healthcare. Primary Health Networks remain key to driving this shift but require dedicated funding, beyond their limited discretionary allocation, for new team-based collaborative models.
Supporting physiotherapists to work in advanced scope roles will provide optimal patient care, working to reduce admissions and readmission rates.
We outline ways to secure significant benefits for patients and the healthcare system. We call for new pathways that maximise the contribution of physiotherapists in inpatient, outpatient and community-based services, in both private and public hospitals. This is where significant gains can be realised; supporting physiotherapists to work at the top of their scope can address current inefficiencies in the hospital sector.
Advanced practice physiotherapists provide a solution to current workforce pressures and future reform must ensure that these roles are prioritised and developed nationally.
New policy paths towards private health insurance reform need to offer more value.
We call for a commitment to preventive strategies, home-based care solutions and addressing the lack of continuity of care for complex conditions. We need to see a reform plan where preventive strategies and management of chronic conditions feature strongly alongside a healthy ageing offering.
Physiotherapists are key participants in providing this vital care and we call for policy leadership to provide certainty of funding based on need and genuine choice on how needs are met.
We outline ways to increase the benefit of physiotherapy in providing vital care for priority populations. Some of the most important areas of care fall within a group of public health insurance areas supporting those with disability, veterans and those affected by workplace injuries. These schemes have proven that they significantly improve lives.
COVID-19 will cast a long shadow with increased pressure on our health system in the years to come—the focus now needs to turn to supporting patients through the unknown of their COVID recovery.
We outline the critical role of physiotherapists in helping COVID-19 patients navigate their recovery. We still have a lot to learn about Long COVID, but we already know that our roadmap back to health will require a strong health workforce response, leveraging physiotherapy to accelerate our recovery. We call for the development of a Long COVID rehabilitation pathway that includes investment in publicly funded physiotherapy to drive new models of care.